What are the 3 types of dialysis vascular access?
1. Fistula
2. Graft
3. Catheter
If you would like to learn more, check out our article on the understanding the types of dialysis access.
What is the difference between a fistula and a graft?
An arteriovenous fistula (AVF) is created by connecting a vein to an artery, typically in your non-dominant arm. Arteries are strong, muscular blood vessels that carry oxygenated blood from your heart throughout the rest of your body, which results in a strong and fast blood flow rate. Veins are blood vessels that return the blood from your body to your heart. They are typically located closer to your skin surface than arteries and easy to reach with dialysis needles. As a result of surgically connecting these blood vessels together, the arterial blood flows into the connected vein and causes the vein to enlarge, which ultimately results in an enlarged vessel that can be used for dialysis.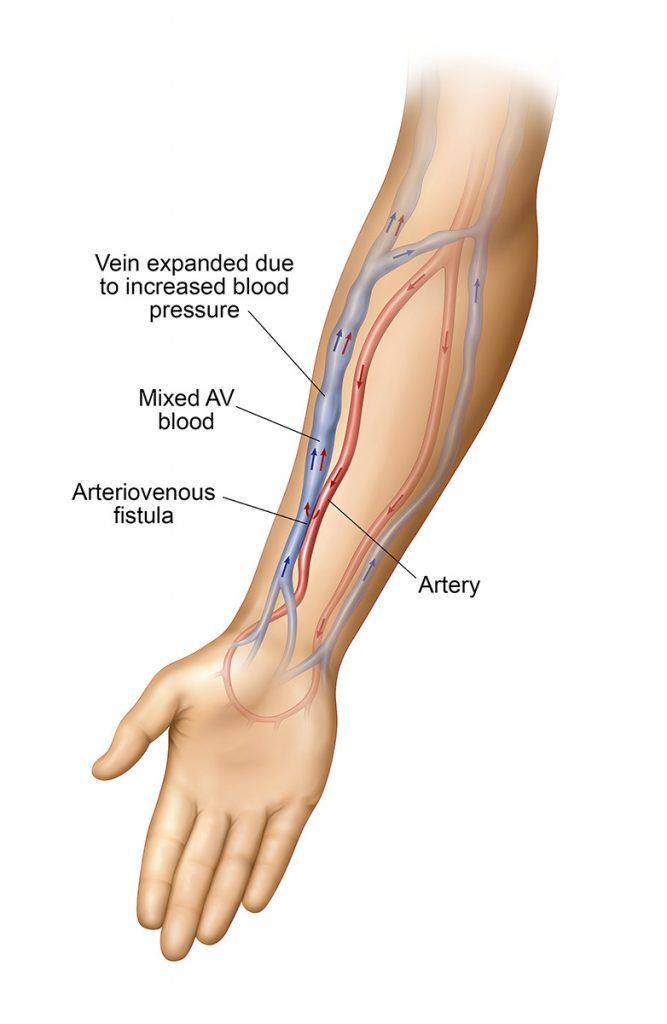
An arteriovenous graft (AVG) is created by using a synthetic tube, usually composed of a specialized plastic, to connect one of your arteries and one of your veins under your skin. One end of the graft is surgically connected to your artery and the other end is connected to your vein. The dialysis needles are inserted into the graft material. Since the graft material is foreign to your body, an AV graft is more likely to get infected than a fistula.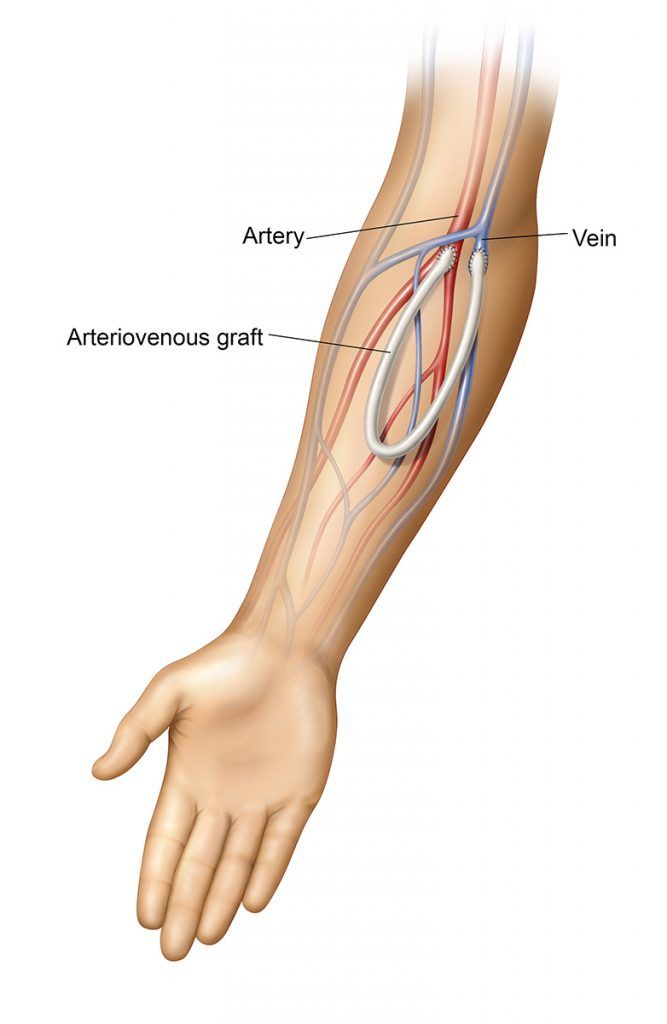
What is the most common problem associated with a fistula or graft?
Narrowing, also known as stenosis, of your blood vessel is the most common problem. This results in an insufficient blood flow through the fistula or graft. Clotting can also cause decreased flow. If you don’t feel a thrill (vibration), your access may be clotted.
What causes the narrowing (stenosis) of a blood vessel?
There can be several causes of stenosis, such as scarring where the artery and vein are sewn together in a fistula or where the artery and vein are connected to the graft. Scars from blood draws may also lead to narrowing of the vein.
How long does it take for a fistula to mature enough so it can be used for dialysis?
After surgery, it takes at least 1 month, although it often takes 3 to 4 months or more for a fistula to mature enough for dialysis.
Can anyone have an AV fistula?
No, unfortunately an AV fistula is not suitable for every patient. Previous needle sticks for IV fluids, blood work, and/or medicines can damage veins over time, creating scar tissue, which can make the creation of an AV fistula impossible. If the veins are damaged, or too small, the AV fistula may not mature. In this situation, other options, include an AVG, or placement of a Central Venous Catheter
Are there complications associated with an AV fistula?
Yes, Some patients may suffer complications such as:
- Infection
- Bleeding
- Arm swelling
- Tingling in the fingers
- Steal syndrome: when the arterial blood doesn’t reach the hand and causes ischemia (lack of oxygen). This condition should be reported to your doctor immediately, and may require an intervention to alleviate the problem or, in some cases, establishment of a new access at a different site.
What are some ways you can improve your chances of having a fistula?
- Ask your doctor to suggest a vascular surgeon who is experienced in fistula creation.
- Ask your doctor about vessel mapping. This painless ultrasound examination lets the doctor see your veins and arteries. Vessel mapping can help your doctor plan an access that will work best for you. It means fewer surprises during access creation.
- Ask your surgeon about a venogram (contrast x-ray of the blood vessels), another way to look at the blood vessels before doing surgery. In many cases a venogram will be performed at the time of the ultrasound evaluation.
What are some of the risks of having a graft?
Grafts may become infected and/or clotted, because the synthetic material is foreign to your body.
After surgery, how long does it take until a graft can be used?
After surgery, it usually takes 3 to 6 weeks before the graft can be used. However, recent advances in the development of graft materials have resulted in the availability of “early stick grafts” that can be used for dialysis within days, rather than weeks, after placement.
Is it normal for my arm to be swollen after graft surgery?
Yes, your arm might be swollen for a short period of time due to tissue trauma from the surgery.
What is a central venous catheter?
A catheter is a plastic tube that is placed in the neck, chest, or groin, and connected to a “central” vein. The other end of the tubing remains outside the skin and used for connecting to the dialysis tubing. Most catheters are temporary, used for weeks or months at most. They are mainly for short-term use, until a graft or fistula is ready. Some patients, however, have a catheter as a permanent access.
Can a catheter for dialysis be used right away?
Yes, catheters can be used the same day for dialysis.
What are the different types of catheters?
- Internal jugular catheter: This is the preferred type of catheter. IJ catheters are less likely to harm blood vessels than another type of catheter, the subclavian. The IJ catheter can be placed so it comes out on the chest and can be hidden by clothing.
- Femoral Catheter: This catheter is placed into the femoral vein, in the groin. Due to its location, the femoral catheter is hard to keep germ-free. As a result, infection is always a risk with this type of access.
How do I take care of my hemodialysis catheter?
Here are a few recommendations for catheter care:
- Keep surgical sites clean and dry until they are completely healed.
- Keep exit sites clean and dry for at least 6-8 weeks.
- If you experience any pain, redness, or swelling at the exit site of the catheter, immediately notify your doctor and/or dialysis nurse.
- Do not pinch, poke, bend, or pull at your catheter.
- Do not use sharp objects around your catheter.
- Do not get your catheter wet (shower, swimming, soaking while bathing) until you have permission from your doctor.
- When in doubt, ask your doctor or your dialysis nurse for advice.
What should I do if my catheter falls out or breaks?
If bleeding occurs, apply pressure to the site immediately. In any event, contact your physician right away since emergency medical attention may be necessary.
Is a tanning salon harmful to my catheter?
Yes. The UVA rays can degrade the catheter’s material.
Can I shower or swim with my catheter?
The CDC recommends that the catheter not be submerged in water, and it is not recommended to swim, shower, or soak catheter dressings while bathing. Contact your physician or dialysis nurse for additional recommendations.
What are possible side effects of having a catheter?
Catheters extend outside of the body, so it is the vascular access type most prone to infection and it is so close to the heart that infections can be serious. Catheters also have a high tendency to clot.
How can a corrective procedure help if I have narrowing (stenosis) in my fistula or graft?
The corrective procedure, called angioplasty, will widen the narrowed portion of the blood vessel and improve flow. If your access is clotted, a procedure called a thrombectomy can be performed to remove the clot(s). Typically these procedures take about 45-60 minutes to perform.
Why is it important to rotate my needle sites?
Your dialysis center’s staff should be using a cannulation technique of rotating your needle sites. They should insert your needles into different places than your last treatment. Rotation of your needle sites will help to prolong the life of your vascular access. Repeated insertion of a needle into the same place causes the wall of the vein to weaken and may result in the formation of an aneurysm (a bulging in the vessel wall).
What are some easy tips to remember to care for my access?
- Keep your access clean and wash it with soap and water every day, particularly just prior to a dialysis treatment.
- Avoid scratching, coughing or sneezing on your access to minimize the risk of infection.
- Avoid clothing with tight armbands, constrictive jewelry, sleeping on, or carrying heavy objects with your access arm.
- Don’t let anyone but your dialysis staff touch your access.
- Your access arm should not be used to check blood pressure, draw blood or place an intravenous line.
- If you do not feel the vibration (thrill) or hear the sound (bruit) in your access, call your physician or dialysis center immediately.
- Redness, swelling, numbness, weakness, bleeding or oozing in your access arm should be brought to the attention of your dialysis caregivers immediately.
What techniques should I know? When should I ask for help?
- If your needle site begins bleeding after you’ve left the dialysis unit, take a clean gauze pad and press directly on the site where the needle was for 15 minutes without peeking. If you peek frequently, it will take longer to clot.
- NOTIFY YOUR DIALYSIS CAREGIVER IMMEDIATELY IF YOU ARE NOT ABLE TO STOP THE BLEEDING.
- If you have a catheter, make sure your dialysis nurse educates you on good catheter care, including cleaning and emergency care in the event the catheter becomes dislodged.
What if my access is no longer functioning well?
You may require an interventional procedure to correct the problem, improving the function of your access. Depending upon why your access is no longer functioning well, you may be referred to a vascular specialist who may correct the problem with a minimally invasive, image-guided procedure.