Sometimes, even when you take the best possible care of your access, there are times when an AV fistula fails. While this can certainly be frustrating and disappointing for the patient, there are fortunately a variety of different treatment options for a malfunctioning or completely failed fistula.
The sooner a failed fistula can be fixed, the quicker you can resume dialysis treatments as normal, so you can remain healthy and feel your best. If your fistula cannot be quickly fixed, your doctor may suggest a temporary access so you can still receive dialysis while your medical team works to have your fistula functioning again.
Let’s explore some reasons as to why a fistula can fail as well as some of the potential treatment options.
What Can Cause an AV Fistula to Fail?
An AV fistula can fail when there is a narrowing, also called stenosis, in one of the vessels associated with the fistula. When a narrowing occurs, the volume and rate of blood flow can decrease, and you may be unable to dialyze adequately.
A fistula can also fail if a blood clot forms in the vessels and blocks the flow of blood, which can prevent dialysis with the AV fistula altogether. (i)
Treatment Options When an AV Fistula Fails
- Medications
- Thrombectomy
- Angioplasty with or without stenting
- Surgical revisions of a failed AV fistula
- Surgical creation of a new fistula
When an AV fistula fails, the sooner it can be tended to the better the outcome can be. Keeping your access working well will help you get the most from hemodialysis, and help you feel your best.
Depending on your specific situation, there are a few treatment options for fistula failure.
Medications
If your AV fistula malfunctions or fails due to the presence of blood clots, your doctors may suggest certain medications depending on the severity of the clots.
Some medications can help thin the blood and dissolve blood clots so that the fistula can function again properly. There are contraindications for using blood thinning medication in some patients, so your doctor will discuss this possibility with you beforehand.
These types of medications can be used on their own, or in conjunction with procedural approaches as described in more detail below. (i)
Thrombectomy
Another option for restoring the functionality of your AV fistula is through a procedure called a thrombectomy. This type of procedure can be completed in the hospital or an outpatient setting.
During a thrombectomy, the physician makes an incision into the blood vessel and passes a small line, called a catheter, to the location of the clots. Once the catheter is in place, the clot can be dissolved by delivering medication directly into the clot. This is called thrombolysis.
Alternatively, the physician can also position a mechanical device at the site to break and remove the blood clots manually. This is referred to as a thrombectomy. (ii,iii)
Angioplasty With or Without Stenting
If a narrowing or blockage is causing your fistula to fail, an angioplasty is another type of procedure used to open up the blood vessels and restore blood flow. This procedure is most often performed under conscious or moderate sedation in an outpatient ambulatory vascular center.
The procedure is done by:
- Threading a thin tube, called a catheter, through a small puncture in the access arm.
- The catheter is then passed through your blood vessel under image guidance until it reaches the area of narrowing or blockage.
- Once in the proper position, a small balloon located at the end of the catheter is inflated, pushing the clots up against the walls of your vessel and opening up the vessel to restore flow.
- After the narrowed or blocked area is successfully widened, the balloon is deflated and removed.
In some cases, a collapsible stent is lined or coated with clot-busting medication and is mounted over the deflated balloon before insertion. When the balloon is inflated, it simultaneously pushes the plaque and opens the stent against the vessel wall. The medication helps to dissolve the clot, and the stent remains in this position permanently to help keep the vessel open. The balloon and wire are then removed. (iv)
Surgical Revisions of a Failed AV Fistula
In some cases, a failed fistula may benefit from a small surgical revision. A variety of imaging tests may be ordered before your doctor suggests this approach to ensure your fistula is suitable for a revision. (i)
Surgical Creation of a New Fistula
If your fistula cannot resume functionality with medication, angioplasty, stenting, or revisions, your doctor may suggest creating a new AV fistula. If the doctor decides that it’s best to create a new vascular access, he or she will create it in a place in the arm above the current fistula. If this isn’t possible, your doctor may want to use the other arm if the vessels are suitable, or he or she might consider creating a fistula elsewhere in the body, such as in the leg. (i)
If you need a new fistula, or if at any time the period between your dialysis treatments is too long, your doctor may suggest placing a temporary access such as a central venous catheter (CVC).
What Are Possible Warning Signs that My AV Fistula Could Be Failing?
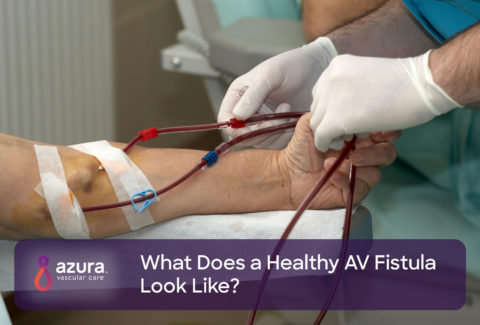
It’s important to be aware of signs that your AV fistula could be failing in order to have the best possible outcome. Your medical team is responsible for monitoring your AV fistula, but you can also play a part in your care and help to spot potential problems early.
Your doctor or nurse will teach you how to feel for the thrill, or bruit, associated with a functioning AV fistula. If at any time this thrill feels weaker than normal or if the thrill has disappeared entirely, it is important to call your physician. Your dialysis team will also monitor your fistula during dialysis treatments to ensure that proper blood flow rates are being met and to assure that you are receiving an adequate dialysis treatment.
If your access is not working well, it can decrease the amount of fluid and toxin removal your dialysis treatment achieves. This, in turn, can affect your overall health and how you feel.
If you suspect there’s a problem with your fistula, notify your dialysis care team right away. You may be referred to an outpatient vascular access center that offers same day or next day appointments so you can avoid hospitalization and missing a scheduled dialysis treatment.
Sources:
(i) National Kidney Foundation. (n.d.). Hemodialysis Access: What you need to know. Retrieved on September 10, 2019 from https://www.kidney.org/sites/default/files/docs/hemodialysis.pdf
(ii) University of Rochester Medical Center. (n.d.). Surgical Thrombectomy. Retrieved on September 10, 2019 from https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=135&contentid=372
(iii) Radiology Info. (January 23, 2019). Dialysis and Fistula/Graft Declotting and Interventions. Retrieved September 10, 2019, from https://www.radiologyinfo.org/en/info.cfm?pg=dialysisfistulagraft.
(iv) Radiology Info. (February 26, 2019). Angioplasty and Vascular Stenting. Retrieved September 10, 2019, from https://www.radiologyinfo.org/en/info.cfm?pg=angioplasty.