When your kidneys are healthy, they work to clean your blood and remove toxins and extra fluid in the form of urine. If faced with chronic kidney disease (CKD), a slow, progressive loss of kidney function, over time it can lead to waste buildup, high blood pressure, anemia, weak bones, poor nutritional health and nerve damage. If CKD progresses and kidneys are no longer able to remove enough of these wastes and fluids from your blood to keep you healthy, you may need dialysis. End-stage renal disease (ESRD) is the progression of CKD to the point where dialysis or transplantation is necessary to sustain life.
Before you can receive dialysis, you must first have a dialysis access created or placed. Your dialysis access is critical to obtaining the best treatment possible, so it is important to understand the different access options. This article will help you understand when to start planning for your dialysis access, the different types of dialysis access, as well as guidelines and tips for your dialysis accessing planning.
Chronic Kidney Disease: When is Dialysis Necessary?
CKD involves the gradual loss of kidney function, which may eventually lead to the need for dialysis. There are five stages of CKD, ranging from stage 1 (kidney damage with normal kidney function) to stage 5, also known as end-stage renal disease (kidney failure).
If you are diagnosed with CKD, your nephrologist, or kidney specialist, will manage your care and monitor your lab work as well as any symptoms closely.
A blood test will determine your glomerular filtration rate (GFR) which tells your doctor how much kidney function remains. If your GFR is low, this means your kidneys aren’t working as well as they should. Your doctor may also order additional lab studies for analysis, which may reveal additional abnormalities that point to advanced stages of chronic kidney failure.
A GFR <15 indicates kidney failure and will require dialysis. When you reach end-stage renal failure, this means that you’ve lost 85-90% of your kidney function. (ii)
You may also experience physical symptoms such as nausea, vomiting, swelling, shortness of breath, fatigue, and weakness. (i) The presence of these symptoms may also prompt your doctor to suggest dialysis access planning.
It is important to note that you can have chronic kidney disease even if these symptoms are not present. (iii) With your lab work and symptoms, your doctor will help you determine the best time to start dialysis access planning, which is usually during mid to late-stage kidney disease.
Planning Dialysis: Types of Dialysis Access
There are two types of dialysis: Hemodialysis and peritoneal dialysis.
If your doctor recommends hemodialysis, an artificial kidney, or dialyzer, will work to remove waste and fluid from your blood. Hemodialysis treatments are scheduled three times per week in-center at a dialysis clinic or home dialysis can be an option for some. During hemodialysis treatments, in order to move blood to and from the body to the dialysis machine, a vascular access needs to be created, also known as hemodialysis access.
The two preferred types of hemodialysis accesses are arteriovenous fistulas (AVF) or arteriovenous grafts (AVG).
To create an arteriovenous fistula, a vascular specialist will connect a vein to an artery underneath the skin, usually in your non-dominant arm. This is considered the first choice for dialysis access because it generally lasts longer and has fewer problems such as infections and clotting.
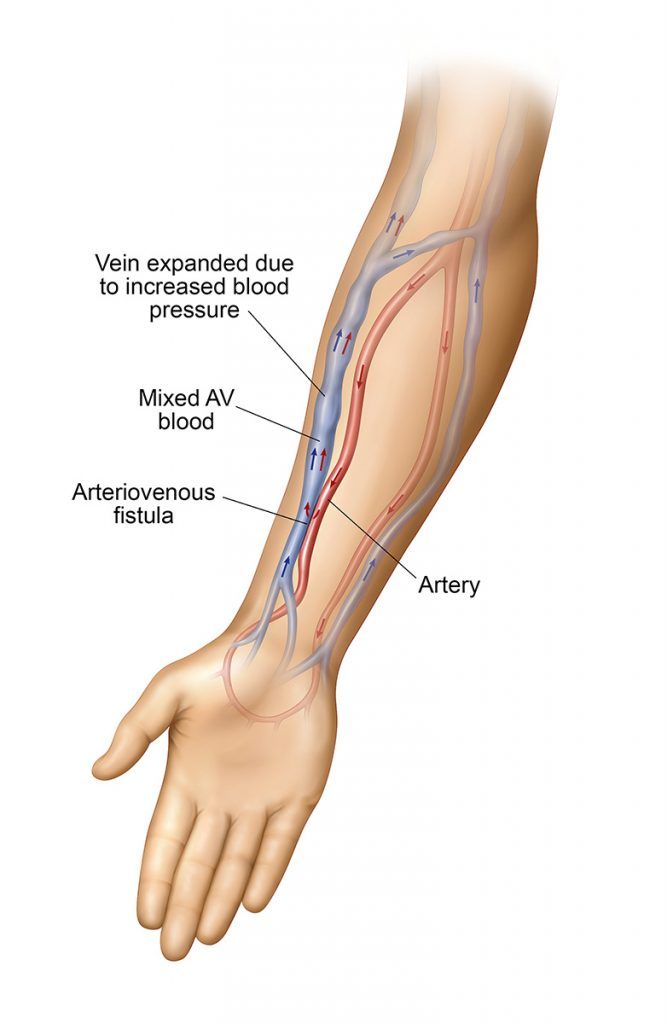
Several weeks before the surgery, your doctor will order a vascular ultrasound exam to measure the size and depth of your veins and arteries in your arms. This is typically referred to as vein mapping or vessel mapping and will help your surgeon determine if you are a suitable candidate for an AVF.
An AVF cannot be used immediately as it needs time to mature after creation and before use, usually a few months. (iv, v)
If for some reason the blood vessels in the arms are found to be of inadequate size for the creation of an arteriovenous fistula, a graft can be placed instead. If this is the case, a soft, flexible biocompatible tube will be placed under the skin, one end is connected to the selected artery, the other to the selected vein, thereby connecting the vein and artery.
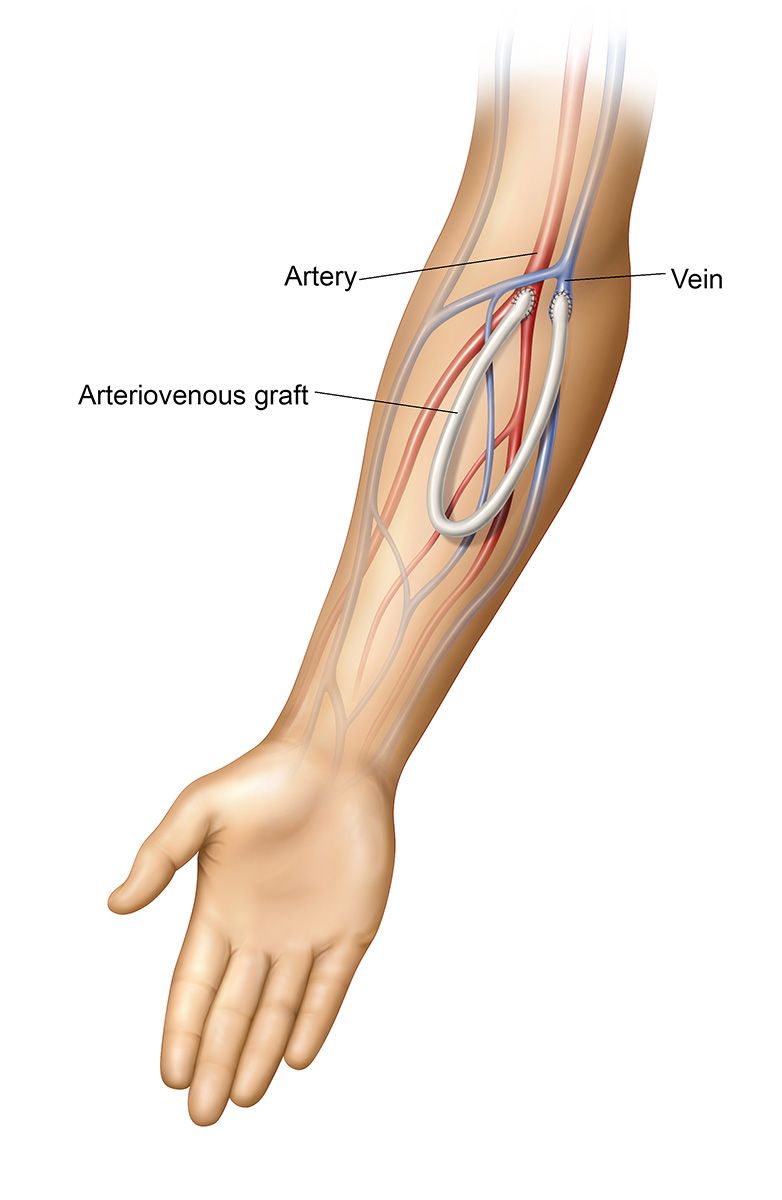
An AVG can be used sooner than a fistula, usually two or three weeks after placement, but it is still the second choice for hemodialysis access because complications are more likely to occur with a graft than a fistula due to the presence of foreign body material (the graft). (iv, v)
A central venous catheter (CVC) is another type of hemodialysis access, but it is typically used in more emergent situations where dialysis is immediately required. With a CVC, a tube is placed within a central vein in your chest with the tip directly in the upper right chamber of your heart. The physician numbs the area of skin for insertion and may use imaging to guide the catheter into its correct location. This type of access is more prone to infection and serious complications and should be avoided if possible. (iv)
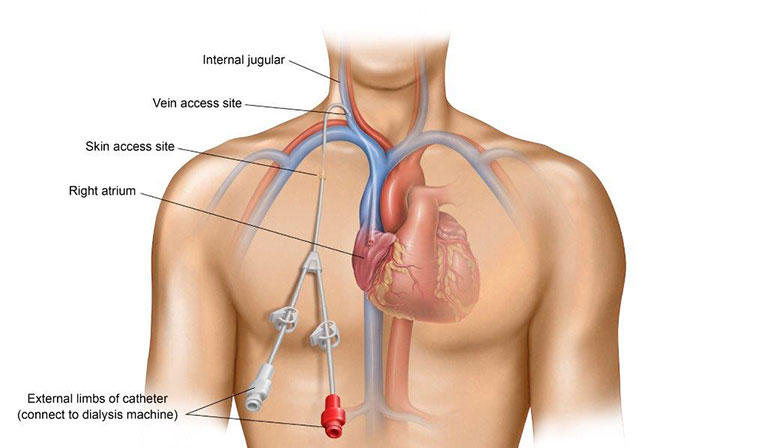
Because AV fistulas and grafts can take time to mature, it is best to be proactive about dialysis access planning and placement in order to avoid having to use a CVC for dialysis.
For some ESRD patients, peritoneal dialysis (PD), is an option that may be recommended by their nephrologist. PD treatments can be performed at home. In peritoneal dialysis, blood does not leave your body like it does with hemodialysis. PD uses your peritoneal membrane – the lining of your abdomen – and a dialysate solution to rid your blood of the toxins your kidneys can no longer eliminate. Before you can receive peritoneal dialysis, you need to have an access, or peritoneal dialysis catheter, placed.
PD catheter placement is a minimally invasive procedure that can be done either in a hospital setting or in an outpatient setting by a vascular specialist.
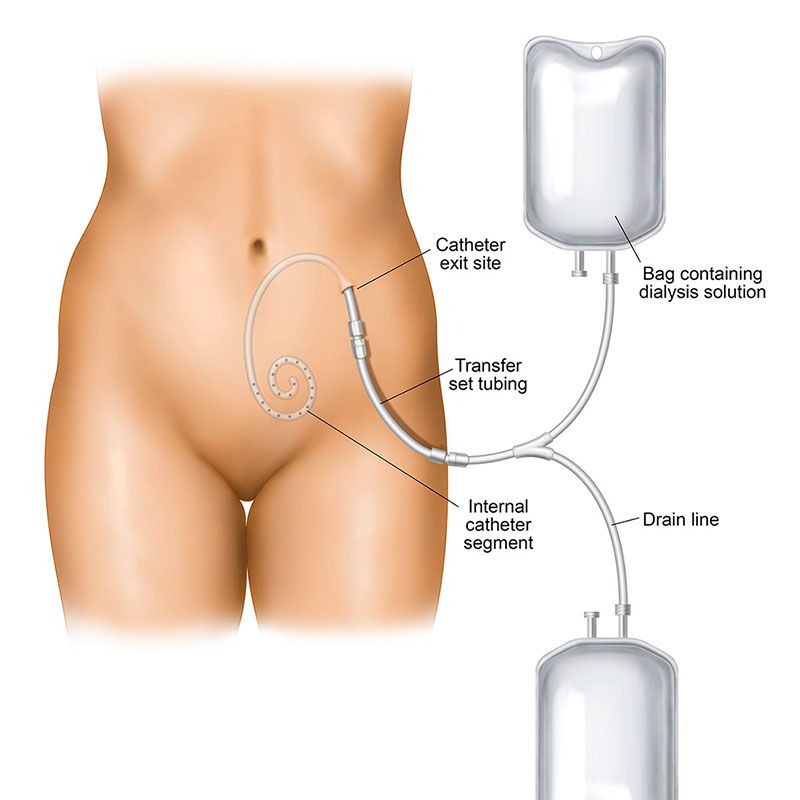
Prior to the procedure, you will be given a local anesthetic, or in some cases a general anesthetic may be used. Your vascular specialist will then make a small incision, where the catheter will be introduced. The catheter is then threaded through a “tunnel,” secured in place, and covered by a sterile dressing over the point where the catheter was placed.
You will likely be able to return home several hours after the procedure, and you may need to take painkillers for a few days following the procedure.
Dialysis Access Planning Steps
If your doctor has determined that your kidney functioning is worsening to the point where you will need dialysis, it is important to work together with your doctor to create a dialysis access plan. Pre-dialysis education is essential in helping you choose the right type of dialysis treatment and dialysis access for you as well as improve your quality of life.
Below is a guideline for dialysis access planning to help you get started. (vi)
My Dialysis Access Plan
| Schedule an appointment with a nephrologist, or kidney doctor, to manage your care
|
While your primary care doctor was likely the first doctor to notice kidney abnormalities in your lab results, nephrologists are specialized in kidney disease and treatment.
Nephrologists can help slow the progression of chronic kidney disease when detected early and will assist in treatment options in later stages, including dialysis access planning.
|
| Determine the type of dialysis treatment | Review with your nephrologist whether hemodialysis or peritoneal dialysis is right for you
|
| Determine the best placement for access | Find the best place for dialysis access by having a vein mapping or vessel mapping ultrasound. This easy imaging test lets your vascular specialist identify the best location and type of dialysis access to create. |
| Meet with the vascular specialist who will create your dialysis access | During this visit, the vascular specialist will explain what to expect before, during, and after access creation and can answer any questions or concerns you might have.
|
| Have dialysis access creation (or placement) procedure | Your dialysis access can be placed by your vascular specialist in an outpatient setting. For hemodialysis, whenever possible, your physician will construct the AV fistula access using only one incision and the AV graft access with only two small incisions.
|
| Wait for your new access to heal | Wait for your new access to heal. The time it takes to heal will depend on the type of dialysis access you’ve received, but your doctor will want to ensure that the access is fully “matured” before it is used.
|
| Using your access | Your care team will determine when your access is fully healed, matured, and ready for use.. If you have any questions during this time, your team is available to help.
|
| Learn to take care of your dialysis access | In addition to keeping the site clean, for an AV fistula or AV graft, learn to feel for the pulse, or “thrill”, with a daily check. Your dialysis team will teach you how to do this, as well as other do’s and don’ts when caring for your access.
|
Sources:
(i) Mayo Clinic. (n.d). Chronic Kidney Disease. Retrieved May 30, 2019, from https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521.
(ii) National Kidney Foundation. (n.d). Estimated Glomerular Filtration Rate (eGFR). Retrieved May 31, 2019 from https://www.kidney.org/atoz/content/gfr.
(iii) National Kidney Foundation. (n.d.). Hemodialysis. Retrieved May 30, 2019 from https://www.kidney.org/atoz/content/hemodialysis.
(iv) National Kidney Foundation. (n.d.). Getting Ready for a “New Normal”: A Helpful Guide for Starting Dialysis. Retrieved on May 30, from https://www.kidney.org/sites/default/files/docs/11-10-
0306_dialysistransitionbk1_oct07_lr_bm.pdf
(v) UCSF Department of Surgery. (July, 2014). Vascular Access for Hemodialysis. Retrieved May 30, 2019 from https://surgery.ucsf.edu/conditions–procedures/vascular-access-for-hemodialysis.aspx.
(vi) Vascular Access Society of the Americas. (n.d). Lifeline for a Lifetime: Planning for Your Vascular Access. Retrieved May 31, 2019 from http://www.vasamd.org/_resources/documents/vascular_access_team/FFCL-Access-Planning-Manual_9natnl-v2.pdf.