When your kidneys are healthy and functioning properly, they work to filter and clean your blood. If your kidneys are no longer able to perform this process on their own, dialysis may be needed to filter your blood and keep you healthy.
If your doctor recommends dialysis treatments due to worsening kidney function, you will first need to have a dialysis access placed in order to receive dialysis treatments.
What Does A Dialysis Access Do?
Simply stated, a dialysis access provides a way to reach your blood during dialysis for cleaning.
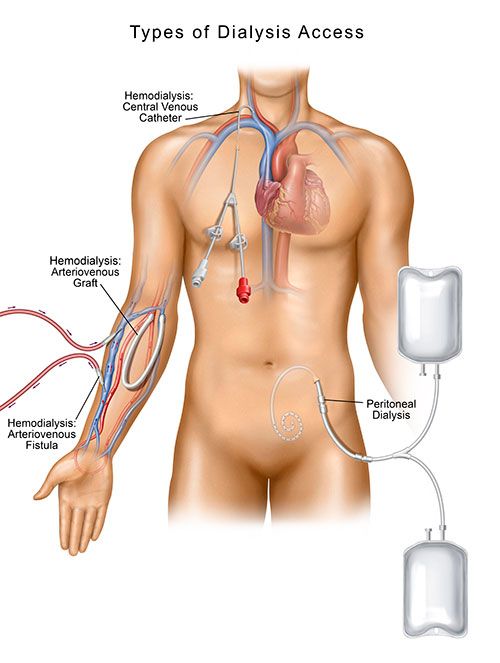
There are two dialysis methods used to treat kidney failure: hemodialysis and peritoneal dialysis. Hemodialysis uses a man-made membrane (a dialyzer) to filter the blood and return it to the body. Peritoneal dialysis uses the inner lining of the abdomen and a sterile solution to filter the blood and remove toxins. Each type of dialysis requires a different way to gain access to your body (in the case of peritoneal dialysis), or your blood for a hemodialysis treatment.
During hemodialysis, a dialysis access allows blood to travel from your body through the arterial blood line to a machine. Connected to is a dialyzer, sometimes referred to as an artificial kidney, and this is where blood is cleaned and then returned to your body through a venous bloodline. While the dialysis machine performs the work of your kidneys, the access serves as the pathway to your blood. (i)
During peritoneal dialysis (PD), an exchange of fluids through a catheter is how the dialysis treatment is achieved . PD is a type of dialysis that uses a person’s peritoneum, the lining of your abdomen, as the filter. A cleaning solution, known as dialysate, absorbs waste and excess fluid from your blood. A peritoneal dialysis (PD) catheter placed in the wall of your abdomen is how the dialysate enters and exits your body.
There are different types of dialysis access, each with their own set of advantages and disadvantages. Let’s explore some of your options.
Different Types of Dialysis Access
There are four dialysis access types.
- Arteriovenous (AV) Fistula
- Arteriovenous (AV) Graft
- Central Venous Catheter (CVC)
- Peritoneal Dialysis (PD) Access
Arteriovenous (AV) Fistula
An arteriovenous (AV) fistula is created by surgically connecting a vein and artery under the surface of your skin, typically in your non-dominant arm. AV fistula creation is a minor surgery performed by a vascular specialist.
When the vein and artery are connected, the higher volume and pressure of blood flow from the artery will cause the vein to enlarge and widen, making it easier to place the needles needed for hemodialysis. This higher flow volume also helps the blood to flow quickly through the dialysis system and back into your body. (i,ii)
When you receive dialysis through a fistula, two needles will be placed in your arm that will connect to the dialysis system through tubing. Your blood flows from your body through the hemodialysis system. The arterial needle removes blood from your body as the venous needle brings cleaned blood from the dialysis system back into your body.
An AV fistula needs time to heal and develop, or mature, before it is ready for use. Typically, this can take a few months. This is why it is essential to work closely with your physician to understand how well your kidneys function and when is the best time to start planning for a dialysis access.
An AV fistula is the preferred access option for hemodialysis. (ii) It is preferred because it usually lasts longer than other access types and is less likely to become infected or malfunction.
Arteriovenous (AV) Graft
Sometimes, a fistula cannot be created. This might be a result of having veins that are too small to support an access, or the blood vessels may have sclerosis, or scarring, from prior needle sticks and IV accesses.
If this is the case, your vascular specialist may place an arteriovenous (AV) graft which is considered a suitable substitute when a fistula cannot be created. An AV graft is a flexible biocompatible tube that makes the connection between your vessels. One end of this tube is connected to an artery and the other end is connected to a vein under the skin. The needles used during hemodialysis are placed directly into the graft material. (i,ii)
An advantage of having an AV graft placed is that it can be used quicker than fistulas. A graft can be used in a few weeks after the site is adequately healed. Grafts, however, are at greater risk to result in an infection or clotting as it is an artificial object that is being placed in the body and your body recognizes this.
Receiving hemodialysis through an AV graft is the same process as receiving hemodialysis through a fistula. During each dialysis treatment, two needles will be placed in your AV graft that will connect to the dialysis system. Then treatment is carried out in the same manner.
Central Venous Catheter (CVC)
A Central Venous Catheter is most often used as temporary access for hemodialysis. The CVC is placed into a large vein, usually in your neck or upper chest. The tip of the CVC rests in the upper right chamber of your heart while the other end of the catheter remains outside of your body. The external portion of the catheter consists of two plastic limbs. One limb is responsible for removing the blood from your body while the other limb returns the cleaned blood to your body. (iii)
There are significant disadvantages to CVC access in comparison to fistulas or grafts. With a CVC, there is an increased risk of serious infection as well as clotting, and you are unable to take a bath or shower without a proper cover over the catheter exit site while it is in place.
The hemodialysis process is slightly different with a catheter than fistulas or grafts. There is no need for needles to take the blood to and from the dialysis system. Dialysis tubing is attached directly to the limbs of your catheter for transport through the dialysis machine.
Peritoneal Dialysis (PD) Access
Peritoneal Dialysis (PD) access is a different approach to dialysis. Instead of using a machine or dialyzer to complete dialysis, peritoneal dialysis uses the inner lining of your abdominal cavity to filter your blood inside your body. (v)
With this type of access, a PD catheter is placed through your skin into the abdominal cavity by a vascular specialist, usually about 2-4 weeks before you start PD. During a dialysis cycle, a solution flows from a bag into your belly via the catheter. Once the solution has finished flowing, your catheter can be capped off, and you are free to move around and resume your normal activities.
At this time, the solution is working to absorb any wastes and excess fluid from your blood. A few hours later, the catheter is uncapped, and the wastes are drained from your peritoneal space into a disposable collection bag. This process is repeated 4 to 6 times every day. (v)
Because PD is completed at home, this type of dialysis access gives a person more freedom than other access types, so patients can typically enjoy a relatively normal life.
You may experience feelings of bloating during the process of exchanging fluids with PD. The major complication of a PD catheter is the risk of infection. Infection usually occurs at the PD catheter exit but can also occur within the tunnel through which the PD catheter passes into the abdominal cavity, and also in the peritoneal space. Peritonitis occurs when bacteria contaminate the peritoneal space. It’s essential to keep the PD catheter site clean and notify your physician immediately of any signs of infection.
When facing dialysis, you ideally want the access type that delivers the best quality of dialysis, the lowest risk for infection, and other complications, and also one that fits in with your lifestyle. Before you need dialysis, talk to your doctor to determine which type of access is right for you.
Sources:
(i) National Kidney Foundation. (n.d.). Hemodialysis Access. Retrieved June 9, 2019 from https://www.kidney.org/atoz/content/hemoaccess.
(ii) Vascular Access Society of the Americas. (n.d). Lifeline for a Lifetime: Planning for Your Vascular Access. Retrieved May 28, 2019 from http://www.vasamd.org/_resources/documents/vascular_access_team/FFCL-Access-Planning-Manual_9natnl-v2.pdf.
(iii) National Kidney Foundation. (n.d.). Hemodialysis Access: What You Need to Know. Retrieved June 10, 2019 from https://www.kidney.org/sites/default/files/docs/hemodialysis.pdf
(iv) Mayo Clinic. (n.d.). Hemodialysis. Retrieved June 11, 2019 from https://www.mayoclinic.org/tests-procedures/hemodialysis/about/pac-20384824
(v) National Institute of Diabetes and Digestive Kidney Diseases. (Jan 2018). Peritoneal Dialysis. Retrieved June 9, 2019 from https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/peritoneal-dialysis.