If you’re on dialysis, you may have either a Central Venous Catheter (CVC), AV fistula, AV graft or PD catheter in place. Caring for your dialysis access is one of your most important jobs regardless of the access type. Your access allows you to receive the lifesaving dialysis treatments you need, but complications affecting your access can delay these treatments. Delays in treatment can have a significant impact on your health. In some cases, access complications can even be life-threatening. Read on to learn how to tell if something is wrong with your access.
Possible Dialysis Access Complications
Each type of dialysis access carries its own risks.
Generally, CVCs are more likely to become infected than fistulas or grafts. [i] CVCs are partly internal with the tip of the catheter resting in the right atrium of your heart. The catheter and its limbs used to access your blood remain external. Bacteria, usually from the skin, can contaminate the external portion of the CVC and eventually migrate into the body causing an infection. [ii]
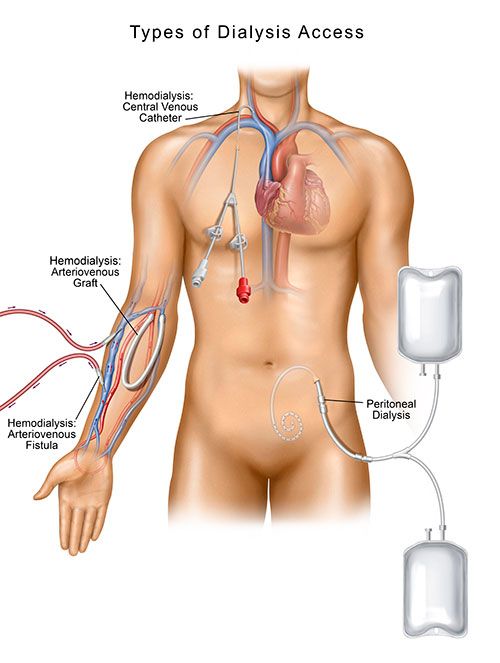
The tip of a PD catheter rests deep in your abdomen and like the CVC, there is a portion of the catheter that remains external. Infections near the PD catheter exit site are common and some infections can even occur inside your abdominal lining or the tunnel that the PD catheter passes through. [iii]
While access infections are less common with fistulas or grafts, any access can become infected. It’s important to remember that people with ESRD often have a compromised immune system. That means that you may be at an especially high risk for all types of infections. All dialysis patients need to watch carefully for signs of an access infection.
Signs of Access Infections
After your access has been placed, check your access area daily for signs of infection. Symptoms of an access infection may include: [iv]
- Pus draining from the access.
- Red streaks around the access area.
- Red, inflamed skin.
- Swelling, warmth, or increased pain.
- Fever.
If you notice any of these symptoms, notify your doctor immediately. Most infections can be resolved with treatment. However, delaying treatment may allow the infection to worsen and spread to other parts of your body.
RELATED: Decreasing Your Risk of an AV Fistula Infection or AV Graft Infection
Signs of Clots
Sometimes an access can become clotted. Clots can block blood flow. They can prevent successful dialysis treatments.
Listen carefully to your AV fistula and AV graft. You should hear a steady swishing sound. This sound is called a bruit, and it’s a sign that your access is working.
If you place your hand over your fistula or graft, you should also feel a vibration. This is known as a thrill. It’s another sign that your access is working the way it should.
Any changes in the bruit or thrill can be a sign that your access is becoming clotted. [v] If you can’t detect any bruit or thrill at all, your access may be completely clotted. Contact your nephrologist right away.
Signs of Catheter Damage
Over time, your CVC or PD catheter may become damaged or broken. Check your catheter access site daily for any of the following problems:
- Swelling
- Bleeding
Examine your catheter for chips, cracks, discoloration, or other signs of damage. Report any damage to your dialysis care team immediately.
How to Prevent Access Complications
Keep it clean
Your dialysis care team instruct you on how to keep your access clean. It’s important to follow all their instructions.
Be gentle
Your access is very important, so be sure to treat it gently. Avoid pulling or tugging on the access if you have a CVC or PD catheter.
After your access surgery for an AV fistula or AV graft, limit physical exertion. Ask your doctor for permission before starting a new exercise program.
Lifting heavy objects can put too much pressure on your access. If you have a fistula or graft in your arm, be careful when picking up items such as grocery bags or large household items. Avoid straining to push or pull anything heavy, such as a piece of furniture.
Check your access bruit or thrill
If you’re on hemodialysis with an AV fistula or AV graft, you’ll need to examine your access daily to check the bruit and thrill. Your dialysis care team can provide detailed instructions on this process. But don’t neglect to perform these checks. If you notice changes in the bruit or thrill, call your nephrologist right away.
See your doctor often
People with ESRD usually have frequent medical appointments. You may need to visit your dialysis center several times a week. You may also have regular appointments with a nephrologist, nephrology nurse, or dietitian. [vi]
Keeping many different appointments can be stressful or inconvenient, but it’s essential that you follow up with all scheduled medical appointments. Your doctor uses your appointment time to check your access for complications. Regular medical appointments ensure that any problems are diagnosed right away. Early detection ensures that you receive the care you need.
What Should I Do if I Suspect That Something Is Wrong With My Access?
If you have any concerns about your access, don’t hesitate to report them to your dialysis care team. The sooner your access problem is treated, the better.
Swift treatment can resolve many common access complications, including infections and clots. Delaying treatment can allow the problems to worsen. If you put off treatment for too long, you may need to be hospitalized. In extreme cases, access complications can even prove fatal.
If you suspect that there’s a problem with your access, notify your dialysis care team right away. You may be referred to an outpatient vascular access center that offers same day, next day appointments so you can avoid hospitalization and missing a scheduled dialysis treatment.
Having trouble understanding your access options? Need more help learning to care for your access? Download our free information sheet, Understanding Your Dialysis Access. Contact your local dialysis care team or nephrologist today for more information. To find the Azura center nearest you, visit our center directory.
Sources:
i Moist, L. M., & Al-Jaishi, A. A. (2013). The Upfront Risks of Vascular Access Complications. Journal of the American Society of Nephrology, 24(10), 1509-1511. doi:10.1681/asn.2013070759
ii Gahlot, R., Nigam, C., Kumar, V., Yadav, G., & Anupurba, S. (2014). Catheter-related bloodstream infections. International journal of critical illness and injury science, 4(2), 162–167. doi:10.4103/2229-5151.134184]
iii Akoh J. A. (2012). Peritoneal dialysis associated infections: An update on diagnosis and management. World journal of nephrology, 1(4), 106–122. doi:10.5527/wjn.v1.i4.106
iv National Kidney Foundation. (2015). Hemodialysis catheters: How to keep yours working well. Retrieved February 26, 2019, from https://www.kidney.org/atoz/content/hemocatheter
v National Kidney Foundation. (2017). A to Z Health Guide, Hemodialysis Access. Retrieved February 26, 2019, from https://www.kidney.org/sites/default/files/11-50-0216_va.pdf
vi National Kidney Foundation. (2016). A to Z Health Guide, Your Dialysis Care Team. Retrieved February 26, 2019, from https://www.kidney.org/atoz/content/dialcareteam