Peripheral Artery Disease (PAD) is a serious disease that is underdiagnosed and undertreated. Many people believe that pain in the legs or lower extremities is just another sign of aging, not realizing that it may be a warning sign for PAD. If left untreated, PAD can progress and lead to severe leg pain and suffering, the death of tissue (gangrene) and limb amputation. PAD can also increase the risk of heart attack and stroke.
Peripheral Artery Disease affects nearly 10 million Americans yet many know little about it. This is why awareness and educating Americans about this disease is so essential. September is Peripheral Artery Disease Awareness Month. It is a time to draw attention to:
- Understanding risk factors for PAD
- The importance of getting diagnosed
- Why getting treated sooner than later makes a difference
What You Need to Know About PAD
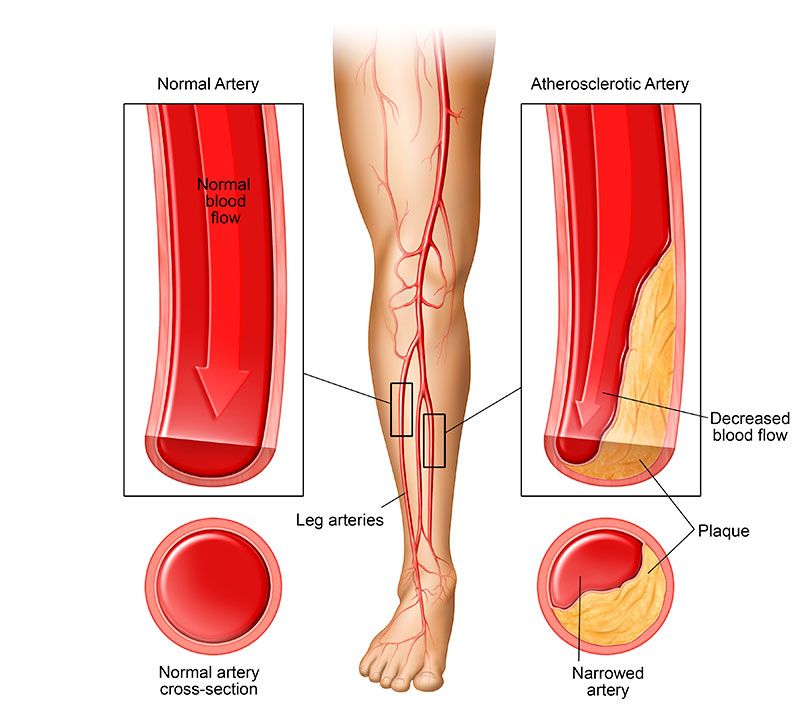
PAD is a chronic disease caused by atherosclerosis, a hardening of the arteries from the buildup of cholesterol and fat, or plaque, in the inner lining of the arteries. This buildup occurs gradually and causes blockage of the arteries, resulting in decreased blood flow and oxygen to the limbs.
While many patients with PAD experience no symptoms, some may have noticeable symptoms such as fatigue, cramping or pain in the legs when walking or moving, which is relieved with rest. This pain or discomfort is claudication, which can be mild or severe. In severe claudication, the pain can be felt even at rest. Other serious symptoms that should not be ignored include discoloration of the lower extremities, poor nail growth on toes, and sores or wounds on toes, feet or legs that do not heal.
Are You at Risk?
For Americans older than 50, there is a one in 20 chance of having PAD. Cigarette smoking, advanced age, high cholesterol, diabetes, high blood pressure, obesity, physical inactivity, kidney failure, family history of vascular disease, and being of African American descent increases the risk for PAD.
If you are older than 50, experiencing leg pain and have more than one of the previously mentioned risk factors, talk to your doctor about PAD and take the PAD Risk Assessment. If you are experiencing any serious symptoms, talk to your doctor as soon as possible.
The Risk of Amputation Is Real
Vascular disease, including PAD, is now responsible for 80 percent of all amputations.1 Unfortunately, too many PAD patients undergo limb amputations, especially those with chronic kidney disease (CKD) and diabetes.
Patients with CKD appear to have an increased incidence of PAD compared to the general population. Patients with decreased kidney function should be aware of this very serious association between CKD and PAD and get screened at the first sign of any PAD symptoms as they are more likely to develop severe PAD that requires amputation.1 Timely clinical intervention is critical to alleviate symptoms and prevent further progression of the disease.
Patients with diabetes, a major risk factor of CKD, tend to have multiple chronic medical conditions, such as high blood pressure or high cholesterol. Additionally, individuals with diabetes are prone to neuropathy, or damage to the peripheral nerves that cause numbness and weakness. It’s important for diabetics to check their feet daily for non-healing ulcers since, due to neuropathy, they may be unable to feel the pain of sores and wounds. Diabetic patients experiencing symptoms of PAD should talk to their doctor immediately.
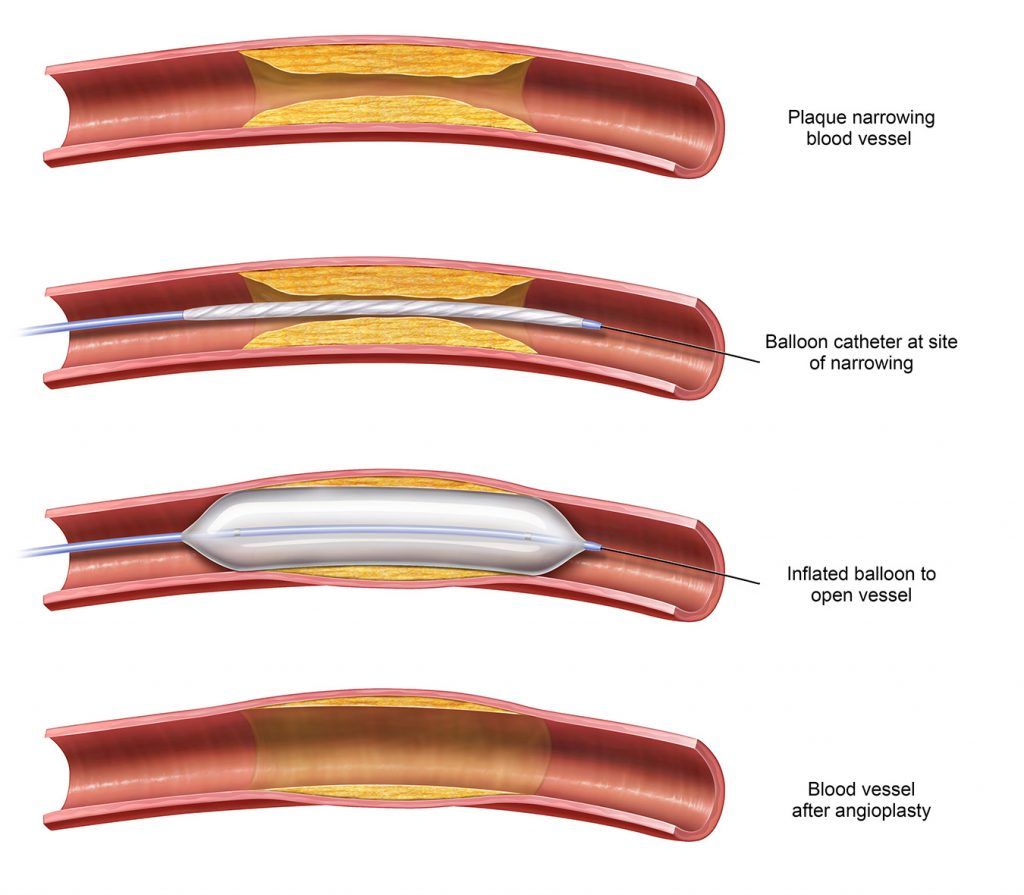
Undergoing an amputation due to advanced PAD is both physically and emotionally devastating—and can be a source of lifelong pain, impact a patient’s quality of life, and the ability to work and function independently.1 Fortunately, there are several treatment options, known as revascularization procedures, that help to restore critical blood flow to the affected limb. These procedures have helped decrease the incidence of major amputations:
- Angioplasty – minimally invasive procedure to improve the blood flow in the vessel
- Atherectomy – minimally invasive procedure that removes the plaque within the vessel
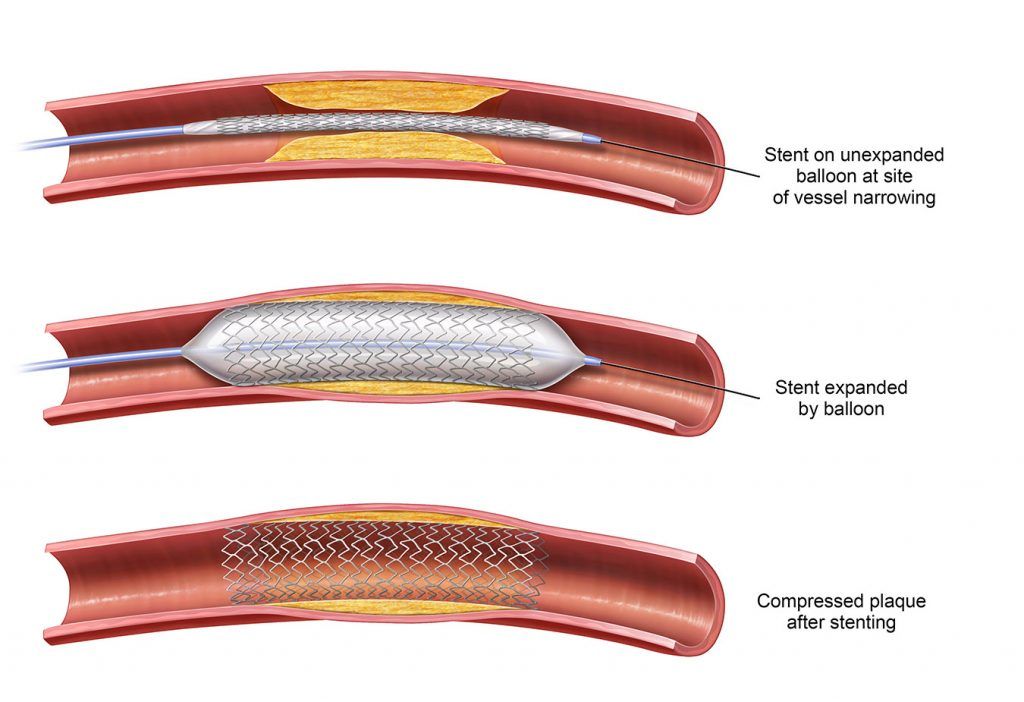
Sometimes stents are used with balloon angioplasty or atherectomy procedures to help hold the affected artery open, aiding circulation in the vessel. A stent is a small, metal mesh tube that is placed in the blocked or narrowed artery and remains in place after the procedure.
Being aware of PAD and knowing the signs and symptoms to look for are important. Even more critical for preventing further progression of PAD and limb preservation is timely clinical intervention: referral to a vascular specialist and PAD treatment. Timely PAD treatment can help decrease the incidence of major amputations by 75 percent.1
PAD Diagnosis
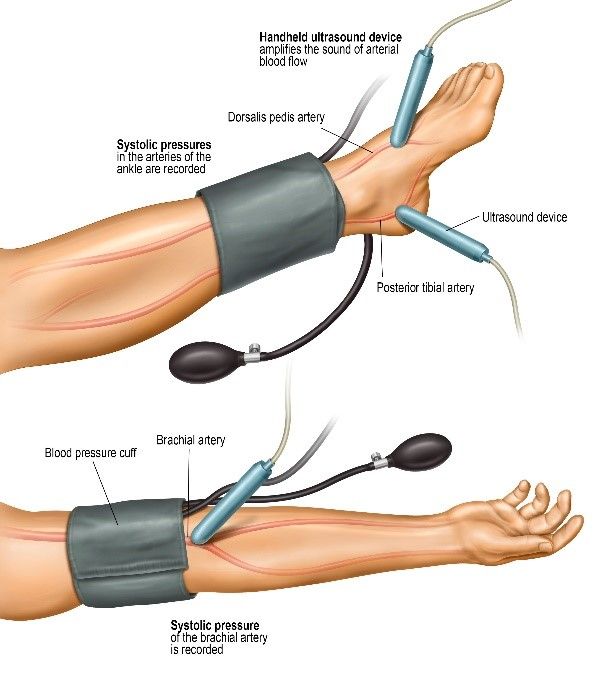
If you experience any symptoms of PAD, talk to your doctor. In addition to a physical exam, a simple, non-invasive test such as ankle brachial index (ABI) may be performed to help determine the presence and severity of PAD.
PAD Treatment
The best treatment for PAD is prevention. Start with a healthy lifestyle: stop smoking, become more active, exercise daily and eat nutritious foods. Beyond that, daily aspirin therapy or other medication prescribed by your physician may prevent complications that may stem from PAD.
For more advanced cases of PAD, angioplasty, atherectomy, stenting or surgery may be needed.
If you have been diagnosed and suffer from PAD, talk to a doctor to help determine the best treatment option for your individual needs. Search for a PAD doctor near you.
Sources:
i Carr, Jeffrey (July 2017). How kidney disease, peripheral artery disease, and amputation intersect. Nephrology News & Issues.