If you have a feeling of heaviness in your leg, mild to severe leg pain after exertion or with rest, or sores on your legs or feet that won’t heal or are slow to heal, you may be suffering from peripheral artery disease (PAD).
What Is Peripheral Artery Disease?
PAD is a progressive disease, meaning it worsens over time if left untreated. PAD is caused by narrowing or blockages of the arteries in the peripheral arterial system, or the arteries in the limbs.i Although other areas of the body can be affected, PAD most often occurs in the legs.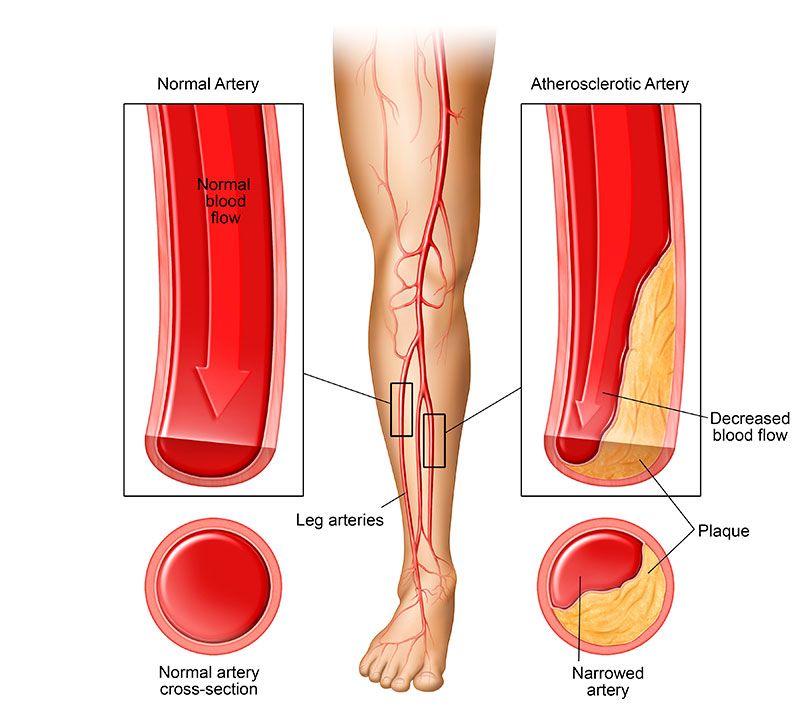
While PAD may start off with mild symptoms resembling leg muscle cramps, the ultimate consequences can be severe. As PAD progresses, less and less blood reaches the lower legs. This can lead to non-healing ulcers, infections, gangrene and even the need for amputation.
Although it can be a devastating disease, there are peripheral arterial disease treatment options available. As with most health problems, early detection is crucial. Take note of the risk factors and symptoms below, and speak with your doctor if there’s any possibility you may have or be at risk of developing PAD. Ask your doctor, “What is peripheral artery disease, and do I have any signs of it?” You’ll find that the tests for PAD are relatively simple and non-invasive, and these examinations just may help to save your legs.
Risk Factors
Some risk factors of PAD are as follows:
Being Over Age 50
As you grow older, your arteries are more likely to form blockages due to accumulation of plaque (fat and cholesterol). This is true even if you have a healthy diet and exercise regularly. Plaque accumulates over time and has a hereditary component. The vast majority of PAD cases are seen in those over 50, and your risk increases as you become older.i You should note, however, that PAD can and does occur in those younger than 50.
High Blood Pressure
If you have high blood pressure, known medically as hypertension, you’re at an increased risk for developing PAD.ii-v Maintaining your blood pressure within normal ranges can help prevent PAD as well as a host of other medical problems. This can be accomplished by following a good diet, getting sufficient exercise and, in some cases, taking medication.
Being of African Descent
African-Americans have an increased risk of several vascular diseases.ii,v This includes PAD. If you are of African heritage, be careful to watch for PAD signs and symptoms.
Having High or Unbalanced Cholesterol
If you have too much LDL (bad cholesterol), and/or too little HDL (good cholesterol), this can lead to artery blockage, including occlusion of the arteries in your lower limbs. This type of artery blockage is one of the main causes of PAD.iii-v You should consult with your primary care physician and keep a close watch on your HDL, LDL and cholesterol numbers.
Being a Type 2 Diabetic
Uncontrolled type 2 diabetes mellitus can ravage your circulatory system. Sustained high blood sugars increase your risk of many kinds of circulatory diseases, including PAD.iii-v While type 2 diabetes is not reversible, keeping your blood glucose levels under control will go a long way towards preventing PAD.
Being a Smoker
We know and understand that smoking is a bad idea for so many reasons. However, it’s never too late to quit. Even if you’ve been a smoker most of your life, smoking cessation has a positive impact on your health and will cut your risk of not only PAD, but a myriad of other health conditions as well.iii-v
Symptoms of PAD
If you have one or more of the above risk factors, understanding the symptoms of PAD is important. Since the disease is progressive, early prevention and intervention is your best chance of minimizing the risk of PAD developing into a dire state or something severely debilitating. The symptoms of peripheral artery disease include:
- Leg fatigue, cramping or heaviness, especially with activity or stair climbing, that often subsides with rest
- Pale or bluish skin tone to the legs
- Leg pain at night or during sleep
- Legs that are cool to the touch
- Decreased hair growth on the legs and feet
- Diminished pulses in the legs and feet
- Wounds, sores or ulcers on the legs and feet that refuse to heal v
Sources:
i Johns Hopkins. Peripheral Vascular Disease. http://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/peripheral_vascular_disease_85,P00236/ (accessed 5/29/2017)
ii Apone, J. “The prevalence of peripheral arterial disease (PAD) and PAD risk factors among different ethnic groups in the US population.” J Vasc Nurs, 2012. 30(2): p. 37-43. https://www.ncbi.nlm.nih.gov/pubmed/22608174
iii Joosten, M.M., Pai, J.K., Bertoia, M.L., Rimm, E.B, Spiegelman, D., Mittleman, M.A., Mukamal, K.J. “Associations between conventional cardiovascular risk factors and risk of peripheral artery disease in men.” JAMA, 2012. 308(16):p. 1660-1667. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733106/
iv Velescu, A., Clara, A., Penafiel, J., Grau, M., Degano, I.R., Marti, R., Ramos, R., Marrugat, J., Elosua, R. “Peripheral arterial disease incidence and associated risk factors in a Mediterranean population-based cohort. The REGICOR study.” Eur J Vasc Endovasc Surg, 2016. 51(5): p. 696-705. http://www.ejves.com/article/S1078-5884(15)00923-5/fulltext
v U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Facts About Peripheral Arterial Disease (P.A.D.). https://www.nhlbi.nih.gov/health/educational/pad/docs/pad_extfctsht_general_508.pdf (accessed 5/29/2017)