Many are familiar with the statistics that high blood pressure and cholesterol can lead to heart disease and stroke. What they can also lead to is a common, yet often undiagnosed condition called peripheral artery disease or PAD.
How Serious of a Condition Is PAD?
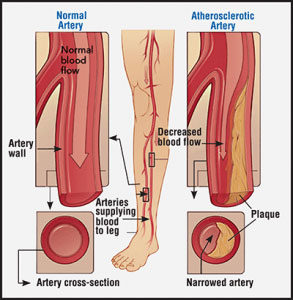
PAD affects one in twenty Americans over age 50 and is a serious condition that if left untreated, can lead to amputation, heart attack, stroke or even death. PAD is a progressive disease, meaning it worsens over time if left untreated. PAD is caused by narrowing or blockages of the arteries in the peripheral arterial system or the arteries in the limbs. (i) Although other areas of the body can be affected, PAD most often occurs in the legs.
While PAD may start off with mild symptoms resembling leg muscle cramps, the ultimate consequences can be severe. As PAD progresses, less and less blood reaches the lower legs. This can lead to non-healing ulcers, infections, gangrene and even the need for amputation.
The Relationship Between High Blood Pressure, High Cholesterol and PAD

Hypertension, or high blood pressure, is a risk factor for many diseases of the cardiovascular system, including PAD. (ii,iii) While everyone has spikes in their blood pressure – during stress or exercise, for example – sustained blood pressures of greater than 120/80 can contribute to PAD. If you have high blood pressure, speak with your doctor about measures you can take to get it under control.
High levels of LDL, or the “bad cholesterol,” can lead to blocked arteries, which is the major cause of PAD. Also, insufficient levels of HDL, the good sort of cholesterol, can be equally damaging and also a risk factor for PAD. Finally, you should keep a close eye on another type of fat that is found in the blood – triglycerides having an elevated triglyceride number is yet another PAD risk factor. (ii,iii)
Other Common Risk Factors For PAD
 Being able to recognize peripheral artery disease risk factors is the first step in preventing the condition. At the very least, knowing these risk factors means you can be diagnosed and treated quickly before more symptoms develop. Some of the most common risk factors for PAD include:
Being able to recognize peripheral artery disease risk factors is the first step in preventing the condition. At the very least, knowing these risk factors means you can be diagnosed and treated quickly before more symptoms develop. Some of the most common risk factors for PAD include:
- Age over 50
- Smoking
- Ethnicity (African American, Hispanic and Native American) (iv)
- Type 2 diabetes
- Family history
Is There a Cure for PAD?
If you have already been diagnosed with peripheral artery disease (PAD), you’re probably asking yourself, “Is there a cure for PAD?” Unfortunately, when your arteries begin to harden, the process can be treated, but not reversed. There is some good news, however. By making healthy changes to your lifestyle and reducing your high cholesterol level, you can help slow the progression of the disease or prevent your PAD from worsening.
Early Detection and Treatment Matters
If you have been diagnosed with PAD and have not started treatment, waiting too long can decrease chances of having a minimally invasive treatment plan as an option and can increase the risk for serious complications, such as chronic infection or gangrene. PAD, if left untreated, may leave amputation as the only treatment option.
If you are experiencing serious symptoms of PAD, particularly non-healing sores on the legs or feet, early detection and treatment for peripheral artery disease matters. It is recommended you speak with your physician about getting screened for PAD immediately. The sooner you are diagnosed and begin PAD treatment, the lower your risk of the disease progressing.
Azura Vascular Care is a national leader in the field of vascular specialty services. Our centers provide safe and comfortable environments with easy scheduling of minimally invasive, outpatient procedures. The vascular specialists and clinical staff at Azura outpatient centers combine medical expertise and compassion to guide you through your PAD treatment journey every step of the way.
If you have been diagnosed with PAD, contact an Azura center to learn more, or request a PAD appointment online.
Sources:
(i) Johns Hopkins. Peripheral Vascular Disease. http://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/peripheral_vascular_disease_85,P00236/ (accessed 5/29/2017)
(ii) U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Facts About Peripheral Arterial Disease (P.A.D.). https://www.nhlbi.nih.gov/health/educational/pad/docs/pad_extfctsht_general_508.pdf (accessed 5/17/2017)
(iii) Joosten, M.M., Pai, J.K., Bertoia, M.L., Rimm, E.B, Spiegelman, D., Mittleman, M.A., Mukamal, K.J. “Associations between conventional cardiovascular risk factors and risk of peripheral artery disease in men.” JAMA, 2012. 308(16): p. 1660-1667. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733106/
(iv) Standing Together Against Limb Loss (Standing TALL) www.togetheragainstlimbloss.com (accessed 09/13/2018)