Peripheral artery disease (PAD) is a serious condition that affects eight to 12 million people in the United States. (i) It is often undiagnosed because people dismiss symptoms as a normal part of aging and do not seek medical care, but prompt treatment can preserve your vascular health and allow you to continue living a normal life.
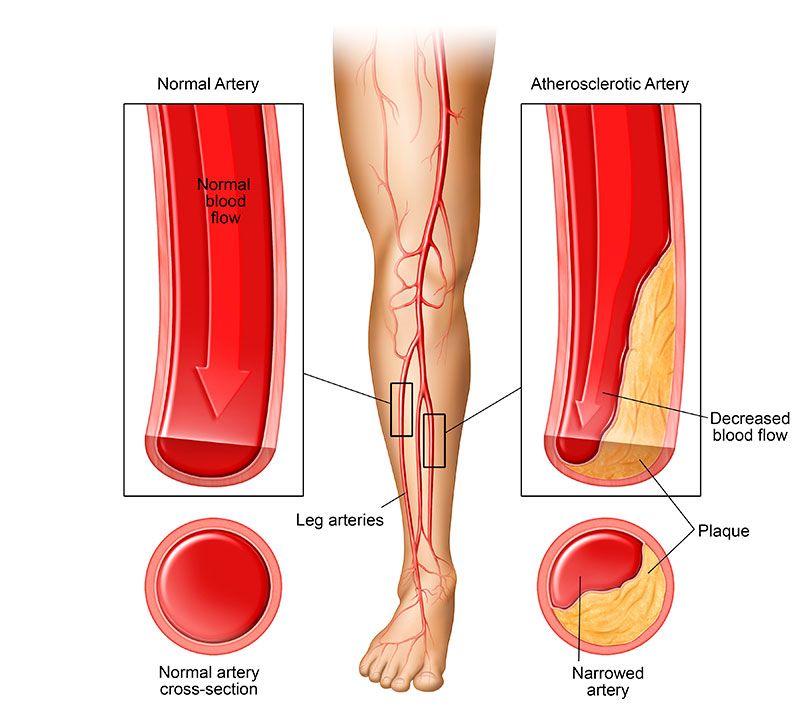
PAD is caused by atherosclerosis, the buildup of plaque on the interior of artery walls. Over time, plaque hardens and narrows arteries, blocking blood flow to the arms and legs. In its early stages, atherosclerosis may not cause any symptoms. By the time you notice the signs of PAD, you might already have significantly blocked arterial blood flow. (ii)
If you suspect that you might have this condition, speak with your doctor or a vascular specialist about getting screened for PAD. Diagnostic tools will be used to measure blood flow throughout your legs and check for any blockages in your arteries. Read on to learn more about diagnosing PAD.
PAD Symptoms
PAD often affects the legs and can cause any of the following symptoms: (iii)
- Leg pain or cramping
- Numbness
- Cold, pale, or bluish skin
- Open sores or wounds
- Slow growing toenails or leg hair
If you notice any of these symptoms, notify your doctor. Ask your doctor what PAD screening tools are available and how your doctor will determine if your symptoms are due to a vascular condition.
PAD Risk Factors
PAD is most common in adults who are 50 years of age or older. Many people with PAD have some of the following risk factors: (iii)
- Smoking
- Diabetes
- Obesity
- High blood pressure
- High cholesterol
- Family history of vascular disease
Although having one or more of these risk factors increases your chances of developing the condition, PAD can affect anyone. About 10 percent of adults over age 55 have PAD. (iv) That’s why it’s a good idea for all older adults to ask their doctors about regular vascular health screenings to check for signs of atherosclerosis.
Diagnosing PAD
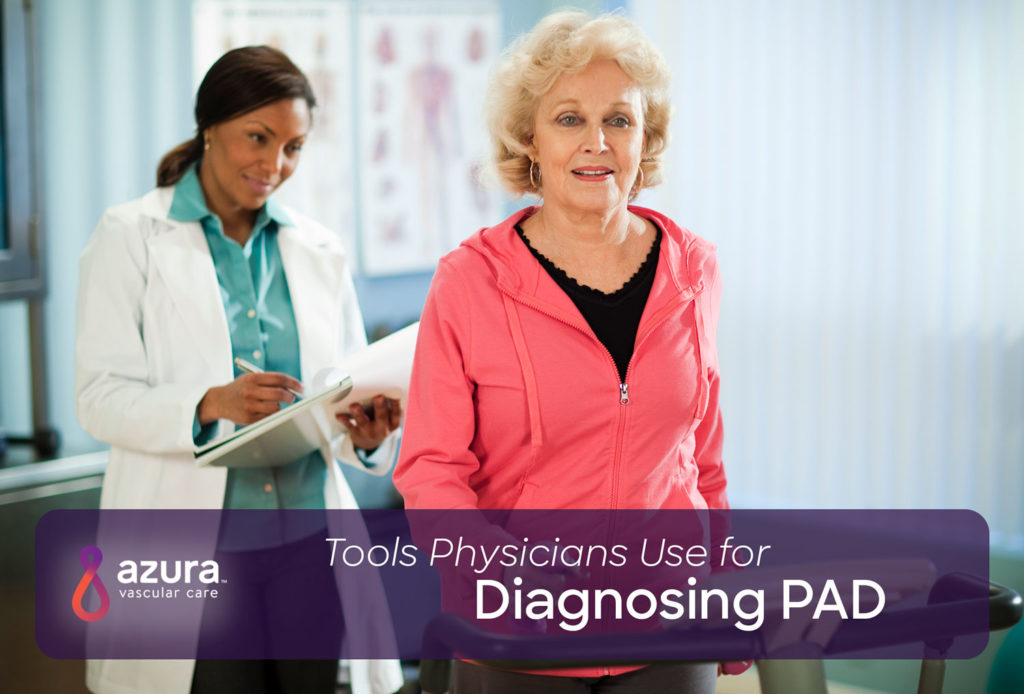
PAD diagnosis begins with a simple physical exam. If the physical exam indicates that additional testing is needed, modern diagnostic tools do an excellent job of helping your doctor determine whether you have PAD.
Ankle-Brachial Index
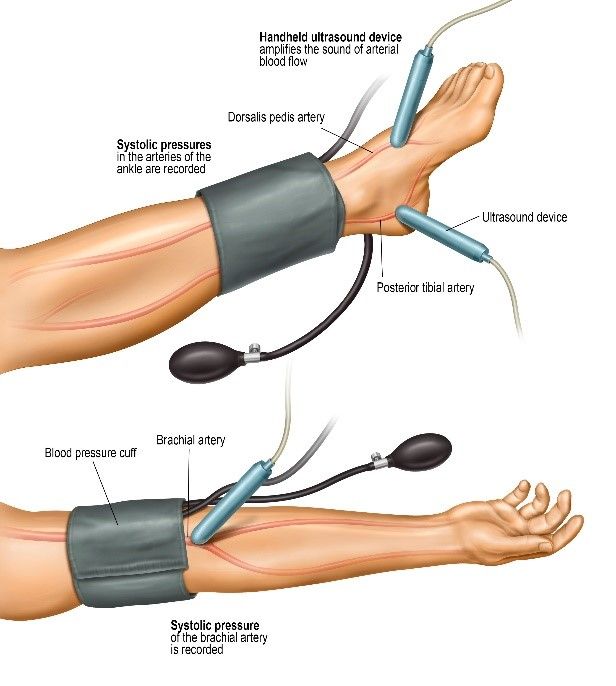
The ankle-brachial index (ABI) is a simple, noninvasive method for checking blood flow in your arms and legs. This test can be performed in your doctor’s office during a routine physical exam.
During the test, your doctor measures the blood pressure in your ankle and the blood pressure in your arm. The two numbers are then compared. (iv) Low blood pressure in the leg may suggest that you have PAD. Depending on the results of this test, your doctor might recommend additional tests for more definitive screening.
Exercise Tests
In some cases, your doctor may have you perform specific exercises before your ABI test. During exercise tests, patients are usually asked to walk on a treadmill for a short time. Then blood pressure cuffs are applied to the arms or legs. (v)
Your doctor uses these cuffs to take several blood pressure measurements. The results of these tests can help determine which arteries might be blocked.
Pulse Volume Recording
A pulse volume recording (PVR) test is another noninvasive test that can be performed in a doctor’s office. A PVR test is usually combined with ABI tests to provide more detailed results. (vi) The test uses a Doppler ultrasound device to create a picture of your blood vessels and arteries. Ultrasounds can help your doctor check for signs of reduced blood flow. (v)
Computed Tomography (CT) Angiogram
A CT angiogram can provide exceptionally detailed images of your arteries. During a CT angiogram, a vascular specialist injects you with a contrast dye. The dye flows throughout your blood vessels and arteries. A CT scan is then performed. Your radiologist reviews the images to see if there are signs of a blockage in your arteries. (vii)
Peripheral Angiogram
Peripheral angiograms are similar to CT angiograms but use an X-ray rather than a CT scan. Like with a CT angiogram, you are first injected with a contrast dye. Next, several X-rays are taken. Your vascular specialist checks the X-rays for signs of narrowed or blocked arteries. (viii)
Treating PAD
Receiving a PAD diagnosis can be frightening. Fortunately, treatment can help resolve painful symptoms and prevent future health complications. Early action is crucial. In its earliest stages, progression of PAD can often be successfully treated through medication or lifestyle changes. The right treatment can help reduce your risk for further complications, including heart attack or stroke. (v)
Treating PAD with Medication and Lifestyle Changes
A variety of prescription medications can help prevent plaque buildup in your arteries. Medication can also help control risk factors like high cholesterol and diabetes. Maintaining a healthy lifestyle is another essential part of managing PAD. Eating a heart-healthy diet, getting regular exercise, and avoiding tobacco can keep atherosclerosis from progressing. (v)
Treating PAD with Minimally Invasive Procedures
Medication and lifestyle changes aren’t always enough to address PAD symptoms, particularly if your arteries are already severely blocked. But even if you have advanced PAD, several treatment options are available. Minimally invasive procedures like angioplasty or stenting can help open up your arteries and restore adequate blood flow. (v)
These procedures can be performed in an outpatient setting including vascular centers. Many PAD patients can take advantage of minimally invasive treatment options and then return home the same day. (ix)
Diagnosing PAD isn’t always easy. If you’re at risk for PAD, it’s important to understand your options for screening and treatment. Take our free PAD risk assessment to learn more about your risk factors and treatment options. Then call 866-534-3627 today to schedule an appointment with a vascular specialist.
Sources:
(i) Facts About Peripheral Arterial Disease (P.A.D.). Retrieved December 11, 2018, from https://www.nhlbi.nih.gov/health/educational/pad/docs/pad_extfctsht_general_508.pdf.
(ii) MedlinePlus. (2018, August 8). Peripheral arterial disease. Retrieved October 22, 2018, from https://medlineplus.gov/peripheralarterialdisease.html
(iii) Mayo Clinic. (2018, July 17). Peripheral artery disease: Symptoms & causes. Retrieved October 22, 2018, from https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
(iv) Mayo Clinic. (2018, January 10). Ankle-brachial index. Retrieved October 22, 2018, https://www.mayoclinic.org/tests-procedures/ankle-brachial-index/about/pac-20392934
(v) Mayo Clinic. (2018, July 17). Peripheral artery disease: Diagnosis & treatment. Retrieved October 22, 2018, from https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563
(vi) Cleveland Clinic. (2013). Pulse volume recordings. Retrieved October 22, 2018, from https://my.clevelandclinic.org/health/diagnostics/17403-pulse-volume-recordings
(vii) RadiologyInfo. (2017, April 1). CT angiography (CTA). Retrieved October 22, 2018, from https://www.radiologyinfo.org/en/info.cfm?pg=angioct
(viii) American Heart Association. (2016, October 31). Peripheral angiogram. Retrieved October 22, 2018, from http://www.heart.org/en/health-topics/peripheral-artery-disease/symptoms-and-diagnosis-of-pad/peripheral-angiogram
(ix) RadiologyInfo. (2018, April 10). Angioplasty and vascular stenting. Retrieved October 22, 2018, from https://www.radiologyinfo.org/en/info.cfm?pg=angioplasty