You used to love taking that morning run around the block. You could work all day and still make multiple trips up and down the stairs to do several loads of laundry in the evenings. Now, all you can think about is the pain in your calves and thighs that just will not go away. Maybe you’ll just sit a little longer…
If you’re experiencing pain in your legs when walking or exercising that disappears when you stop, it may be time to learn about peripheral artery disease (PAD). There are several contributing factors that can lead to PAD—here we’ll discuss some of the major causes and how to prevent the disease, along with some of the symptoms of PAD.
What Actually Causes PAD?
Plaque Deposits & a Lack of Blood Flow
PAD may be causing the pain in your legs and feet, but what actually causes peripheral artery disease is a lack of blood flow. PAD starts when arteries narrow and prevent blood from flowing properly to your legs. The American Heart Association estimates that 8.5 million Americans, most of them older, have been diagnosed with PAD.
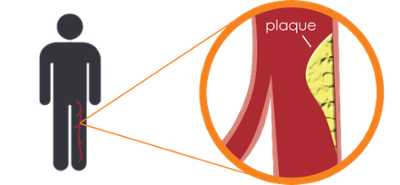
Peripheral artery disease is a symptom of a more severe problem called atherosclerosis, which occurs when arteries outside the heart accumulate deposits of calcium, fat, cholesterol and other materials, what doctors commonly call plaque deposits. The arteries first affected are those supplying oxygen to your legs and feet. These arteries begin to narrow and harden, ultimately reducing blood flow to your legs. Plaque deposits in your arteries can eventually lead to blockage which severely reduces blood flow. This condition, called Critical Limb Ischemia (CLI) can result in sores and wounds that don’t heal.
Doctors haven’t found an exact cause for these plaque deposits in arteries, but there is enough evidence to suggest that several controllable PAD risk factors contribute to the plaque build-up that causes peripheral artery disease, according to the National Institutes of Health.
4 of the Most Common Risk Factors for PAD
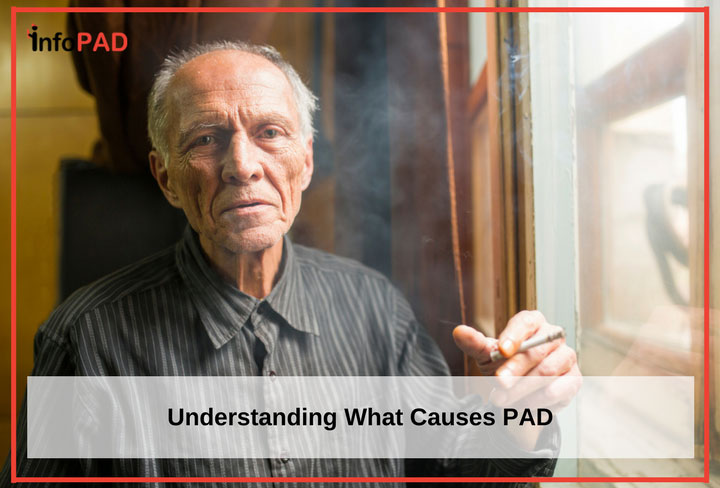
1. Smoking
Smoking is one of the biggest contributors to the onset of PAD. Smoking damages the inner layers of the arteries. Your body attempts to heal itself and plaque builds up in the damaged areas. This could lead to blood clots or “thrombi,” which then adhere to the vessel wall and narrow the space in the artery for blood flow. Smoking cessation has been shown to be effective in eliminating or greatly reducing the effects of PAD.
2. Lack of Exercise
Another strong indicator connected to PAD is lack of exercise. PAD patients should exercise as exercising improves blood flow and helps overall health by reducing blood sugar and blood pressure and lowering cholesterol. Those with sedentary lifestyles are at a higher risk for all of these conditions. Participating in a regular exercise program will go a long way toward reducing this risk.
3. Diabetes, High Cholesterol, & High Blood Pressure
Diabetics are more at risk because high blood glucose (“blood sugar”) counts in the blood are connected to plaque build-up in the arteries. Doctors state that controlling Type II diabetes with proper glucose monitoring, diet, and exercise changes, and perhaps medication, can help reduce the risk for PAD. Patients diagnosed with high cholesterol and high blood pressure are also at risk. Those diagnosed with PAD should work to maintain proper blood sugar levels and keep cholesterol and blood pressure in check. The best way to do this is by maintaining a healthy diet.
4. Blood Vessel Inflammation
A PAD diagnosis isn’t always linked to plaque build-up around the heart. PAD can also be the result of blood vessel inflammation, which also narrows arteries. Some people who’ve had previous injuries to their legs may also be at risk for PAD. Some less common causes of PAD may include radiation exposure and an unusual anatomy of ligaments and muscles.
How to Tell If You May Have PAD
Know the Symptoms
There are some common symptoms of PAD, but it’s important to note that some people have no symptoms at all. While pain in your calves is the most common symptom, patients have also reported pain in their thighs, hips, buttocks, and even feet. The pain typically begins when you’re doing physical activity and is relieved when you rest. The pain is often described as an aching or tightness. It doesn’t feel like a typical pain someone experiences merely from overexertion.
There are other symptoms of PAD, including:
- Your legs feel cold to touch, while your arms are at a normal temperature.
- You have a wound on your leg or foot that just will not heal.
- Your legs look shiny and there isn’t as much hair on them as before.
- In males, erectile dysfunction is an indicator.
What to Do If You Think You May Have Developed PAD or Are at Risk
Speak With Your Doctor
PAD is a potentially life-threatening disease and it’s important to seek peripheral artery disease treatment as soon as possible. Proper treatment can ease pain and, in some cases, even reverse the disease. Treatment is often easy to implement with basic lifestyle changes. If you think you are at risk for having PAD, your next step should be to schedule an appointment with your doctor to discuss your leg pain and symptoms. During your appointment your doctor will perform diagnostic tests to determine if you do have PAD and discuss a proper treatment plan.