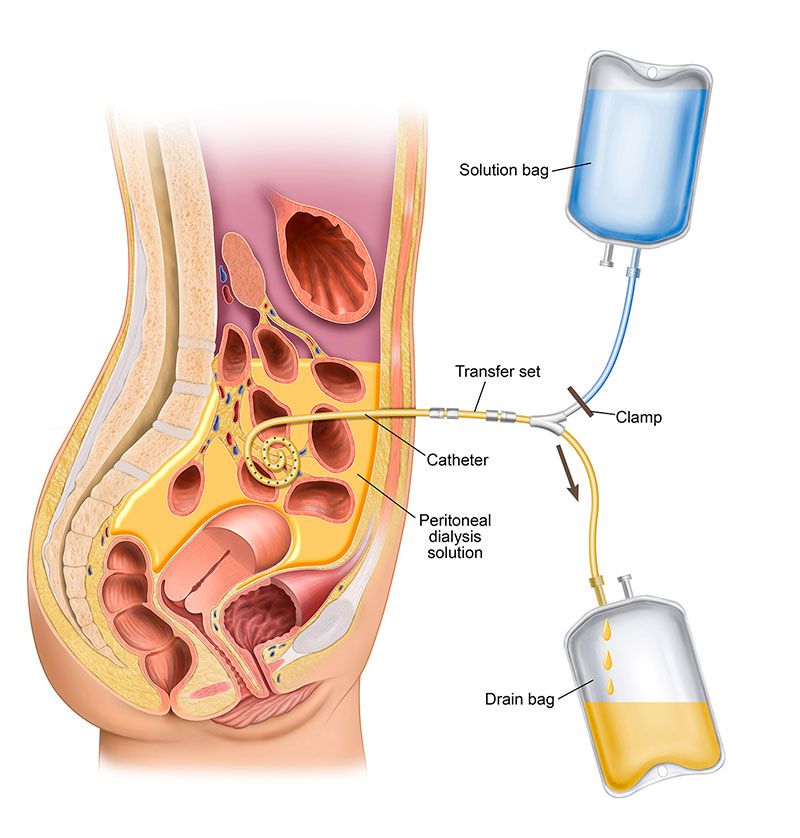
Before you can begin peritoneal dialysis (PD) treatments, you need to have a peritoneal dialysis (PD) catheter placed as an access for the removal of waste and toxins from your body. A PD catheter, the only type of dialysis access used for PD, is placed through your abdomen and into the peritoneal space through the peritoneal membrane—the thin membrane that lines your abdominal wall.
Learning the ins and outs of the placement procedure can help put you at ease. Here’s everything you should know:
What Happens During PD Catheter Placement?
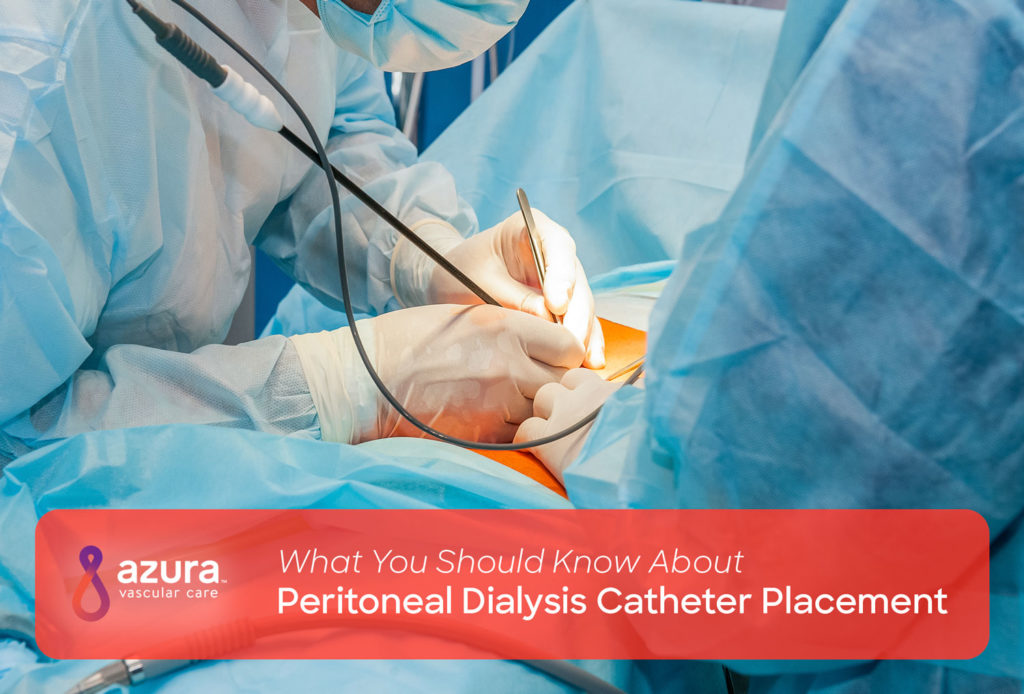
PD catheter placement is typically performed as a minimally invasive procedure in an outpatient setting. Many vascular access centers perform percutaneous catheter placement, which is far less invasive than surgery. Percutaneous catheter placement is performed using fluoroscopy—an imaging technique that uses X-rays to help your vascular specialist view the inside of your abdomen. (i) This procedure requires only local anesthesia and sedation. (i)
Your vascular specialist begins by using a fine needle to make a series of small punctures in your skin to access the peritoneum. (i) The PD catheter is then passed through a small tunnel in your belly into the peritoneum and secured in place.
A PD catheter is made of silicone or another soft, flexible medical-grade material. (ii) Your catheter will have cuffs on it to prevent it from shifting and moving around, and that helps keep bacteria out of the tunnel and exit site. The PD catheter exit site is typically placed to the left or right of your belly button, you should discuss your personal placement preferences with your vascular specialist. (ii) As you recover, your tissue will grow around and fill in part of the exit site as well to prevent the catheter from moving.
After the PD catheter has been inserted, your vascular specialist will place sutures around the catheter on the outside of your abdomen and cover the site with a sterile dressing.
PD catheter placement can usually be performed in under one hour. (iii) However, you may spend additional time in the recovery room before going home so your vascular access team can monitor you for complications after the procedure.
How to Prepare for Your Procedure
Your vascular specialist will give you detailed instructions regarding what you can and cannot do prior to PD catheter placement. Follow your pre-op instructions as closely as possible to reduce your risk for infection and other complications during this procedure.
You may be instructed to take stool softeners within three to four days before your surgery to prevent constipation. (iii) Constipation can interfere with proper functioning of the PD catheter and result in pain when flushing and using the catheter. Taking stool softeners is necessary even if you don’t typically experience constipation since the anesthesia and medications used for PD catheter placement can contribute to constipation. (iii)
Here are more ways to prepare for your catheter placement: (iii)
- Do not consume food or liquids after midnight on the evening before your procedure.
- Follow your doctor’s instructions for using blood-thinning medications if you typically use these drugs.
- Continue using medications as directed with only a small sip of water.
- Arrange for transportation to and from the vascular access center since the medications given during your procedure may make you drowsy.
Learn more about dialysis access surgery here
What to Expect after PD Catheter Placement
You may experience mild pain, discomfort, loss of appetite, and fatigue following PD catheter placement. (iii) All of these symptoms are normal and will eventually resolve on their own within a few days.
Keep your dressing dry at all times and do not shower or expose your access site to water without approval from your doctor. Do not remove the dressing covering your access site, since this could expose your healing wound to bacteria and increase the risk for infection. A vascular specialist will remove the dressing for you at your next appointment.
Continue taking stool softeners for three to four days following your PD catheter placement to avoid constipation. This is especially important if you are taking prescription painkillers since these medications can worsen constipation. (iii)
Contact your doctor immediately if you experience warmth, swelling, redness, or discharge at the access site. These signs can indicate a possible PD catheter infection.
Caring for your PD Catheter
Caring for your catheter is extremely important following its placement since PD is linked to a high risk for infection at the catheter exit site, in the tunnel for the catheter, and in the peritoneum. (iv) This type of abdominal infection is known as peritonitis. (v)
Follow these rules for PD catheter care to reduce your risk for peritonitis:
- Wash your hands thoroughly with soap and water before and after handling your catheter.
- Clean your access site every day to eliminate bacteria.
- Store your dialysis supplies in a clean, dry, and cool place.
- Perform dialysis in clean, dry places that are well lit to reduce contamination risk.
- Wear a surgical mask each time you open the end caps of your PD catheter.
- Thoroughly inspect every bag of solution for signs of cloudiness and contamination before use.
- Avoid wearing tight, restrictive clothing and belts near the access site. (vi)
- Keep sharp objects like scissors away from your catheter at all times.
- Keep the catheter taped against your skin to prevent it from catching on clothing and other objects.
Don’t hesitate to ask your vascular specialist for help and guidance with using and caring for your PD catheter. Proper catheter care can prolong the life of your catheter and help you stay healthy for as long as you need PD.
Questions to Ask About PD Catheter Placement
- How long will PD catheter placement take?
- How soon can I resume bathing, showering, and swimming after my procedure?
- Which stool softeners do you recommend I take before and after my procedure?
- How long will it take for me to heal from this procedure?
- How long does the PD catheter need to stay inside me?
- How is a PD catheter removed?
- Which activities should I avoid while the PD catheter is in place?
- What are the most obvious signs of infection around the exit site?
Azura Vascular Care offers a range of dialysis access care procedures and is devoted to helping you fully understand caring for your dialysis access.
Sources:
(i) Al-Hwiesh, A. K. (2014, March – April). Percutaneous peritoneal dialysis catheter insertion by a nephrologist: A new, simple, and safe technique. Peritoneal Dialysis International. 34(2): 204–211.
(ii) Burkart, J. M. (2018, March 12). Patient education: Peritoneal dialysis (beyond the basics). UpToDate. Retrieved February 14, 2018, from https://www.uptodate.com/contents/peritoneal-dialysis-beyond-the-basics.
(iii) UC School of Medicine Department of Surgery. (n.d.). Peritoneal dialysis catheter placement. Retrieved February 14, 2018, from http://www.ucdenver.edu/academics/colleges/medicalschool/departments/surgery/divisions/transplant/Types-of-Surgery/Dialysis-Access/Pages/Peritoneal-Dialysis.aspx.
(iv) Akoh, J. A. (2012). Peritoneal dialysis associated infections: An update on diagnosis and management. World Journal of Nephrology, 1(4), 106-122.
(v) USCF Department of Surgery. (n.d.). Peritoneal dialysis. Retrieved February 14, 2018, from https://surgery.ucsf.edu/conditions–procedures/peritoneal-dialysis.aspx.
(vi) National Kidney Foundation. (n.d.). Peritoneal dialysis: What you need to know. Retrieved February 14, 2018, from https://www.kidney.org/sites/default/files/docs/peritonealdialysis.pdf.