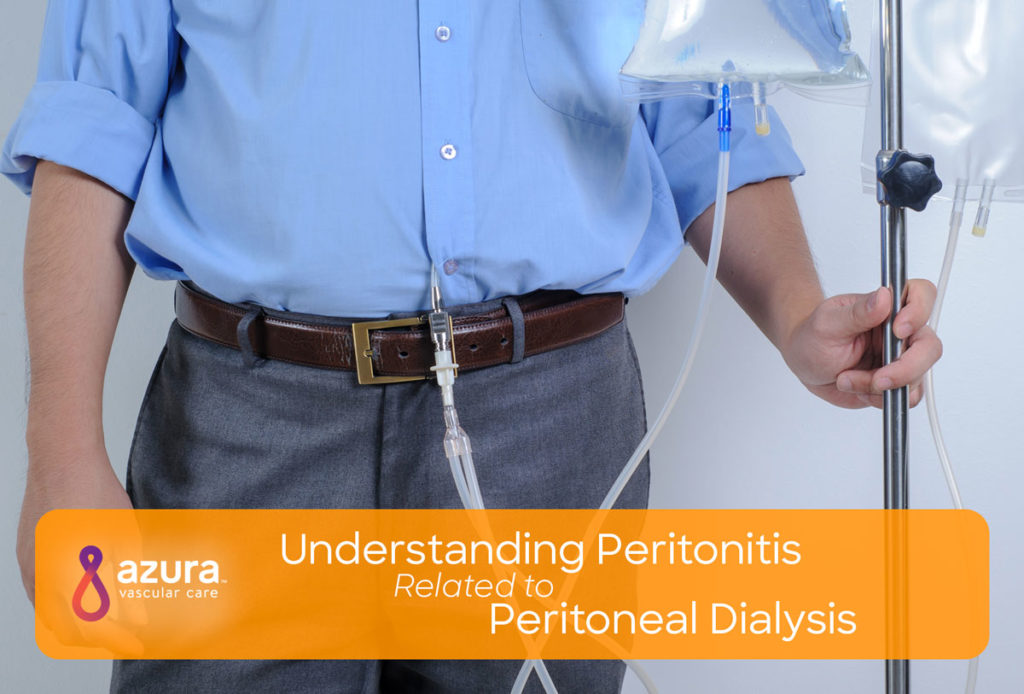
Peritonitis is one of the few complications associated with peritoneal dialysis. The peritoneum is the thin membrane that lines your abdominal cavity and covers the organs contained within it. Peritonitis is the inflammation of this membrane.
Although peritonitis can result from other causes, such as an abdominal injury or appendicitis, this article will strictly focus on peritonitis as it relates to the peritoneal dialysis patient. If you or a loved one has a peritoneal dialysis (PD) catheter, read on to learn more about what causes peritonitis, what can be done to avoid it and how its treated.
What causes Peritonitis in Peritoneal Dialysis patients?
Peritonitis is a peritoneal dialysis-related infection caused by bacteria entering the abdomen from outside the body and infecting the peritoneum. Bacteria may enter the body through the open ends of the PD catheter during exchanges. If you touch your PD catheter cap, bacteria from your fingers may transfer onto the catheter and enter the peritoneum.(iii) Peritonitis can also occur if there is PD catheter exit site infection or tunnel infection.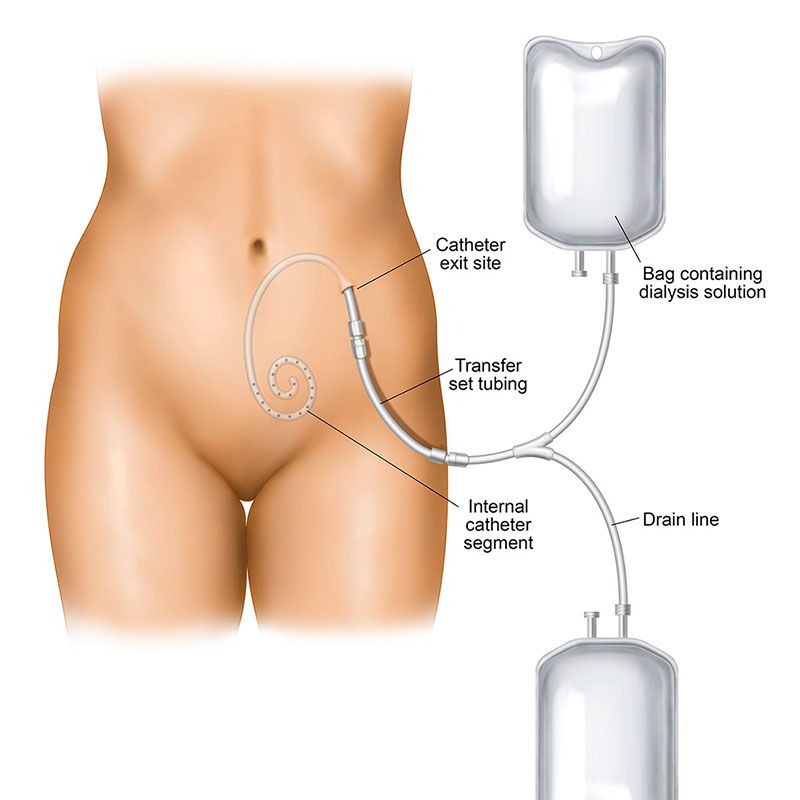
Signs and Symptoms of Peritonitis
As a peritoneal dialysis patient, it’s important to know the signs and symptoms of peritonitis. If you experience any of the following, contact your doctor immediately.
- Abdominal pain
- Fever, nausea, or vomiting
- Cloudy dialysis fluid when drained from your body
- Sore or swollen abdomen
- Redness or swelling at the catheter exit site
- Loss of appetite, fatigue
Diagnosing Peritonitis in the Peritoneal Dialysis Patient
Your doctor may be able to diagnose peritonitis based on your signs and symptoms and status as a peritoneal dialysis patient.
Beyond performing a physical exam, your doctor may elect to analyze a small sample of blood and/or the dialysis fluid taken from your abdomen. Peritoneal dialysis fluid is usually clear but becomes cloudy if peritonitis is present. If the sample shows a high amount of white blood cells, this would indicate an infection.(i)
Treating Peritonitis
Early detection of peritonitis is crucial, as ignoring your symptoms can lead to more serious, life-threatening complications. The sooner you get treated, the better chance you have at keeping the infection from spreading. Peritonitis can be easily treated with antibiotics if caught early and started quickly after the diagnosis. Antibiotics can be added to your new dialysis fluid or be taken as oral tablets.
If peritonitis is not treated right away, you can develop bacteremia, which is a bloodstream infection. Bacteremia, if left untreated, could turn into a systemic inflammatory response syndrome (SIRS), sepsis, or multiple organ dysfunction syndrome (MODS).(ii) Depending on how serious the infection is, hospitalization may be required and you may receive medication for pain, fluid administration through an IV and, depending on the severity of your infection, possibly a blood transfusion.
Catheter removal is also a consideration if you have had repeated bouts of peritonitis. Your doctor may recommend that you receive dialysis in an alternate way until your body recovers from the infection. In any case, your physician will know the best approach for your situation.(iii)
How to Prevent Peritonitis
Peritoneal dialysis-related peritonitis is most often caused by bacteria around the catheter. If you are a peritoneal dialysis patient, prevent peritonitis by following these steps: (iii)
- Keep the skin around your PD catheter clean and check for redness, drainage, or swelling.
- Wash or sanitize your hands before touching the catheter.
- Wear a new surgical mask and gloves every time you care for your access.
- Do not touch an uncapped catheter tip.
- Avoid swimming or taking baths.
- Do not sleep with pets.
Caring for your PD catheter
Care of the catheter and the skin around the catheter (called the catheter exit site) is very important in maintaining PD catheter function and to minimize the risk of developing an infection.
Care after insertion
After the catheter is inserted, the insertion site is usually covered with a gauze dressing and tape to prevent the catheter from moving and to keep the area clean. For the first seven to ten days after the catheter insertion, typically nothing needs to be done to the catheter exit site. The dressing should be left alone and first changed at your PD home training center seven to ten days after placement. If a dressing change is needed before this time, it should be done by a specially trained PD nurse using sterile techniques. The catheter should not be moved or handled excessively, because this can increase the risk of infection.
The area should be kept dry until it is well healed, usually for 10 to 14 days. This means that you should not take a shower or bath or go swimming during this time. A washcloth or sponge may be used to clean the body, although you should be careful to keep the catheter and dressing dry. While healing (two to three weeks), you will be asked to limit lifting and vigorous exercise.
Long term care
After the catheter site has healed, your dialysis nurse will instruct you on catheter exit-site care. It will be important to keep the area clean to minimize the risk of skin infection, as well as peritonitis. In addition, it may recommended that you “anchor” the catheter with tape to stabilize the catheter and minimize the chance of movement causing injury to the healed exit site.
The skin around the catheter site should be cleaned daily or every other day with antibacterial soap or an antiseptic. The soap should be stored in the original bottle (not poured into another container). Other types of cleansers, such as hydrogen peroxide or alcohol, should NOT be used unless directed by your dialysis team.
- Before cleaning the area, wash your hands with soap and water and put on clean gloves.
- Hold the catheter still during cleaning, which helps prevent injury to the skin.
- Do not pick at or remove crusts or scabs at the site.
- Pat the skin until dry around the site after cleaning. A clean cloth or towel is suggested.
- Apply antibiotic cream (if prescribed by your dialysis care team) to the skin around the catheter with a cotton-tip swab every time the dressing is changed.
With appropriate catheter placement and exit-site care, most peritoneal dialysis catheters are problem-free and work well for years.
An infection can happen even when taking the very best care of your PD catheter and adhering to good hygiene. Remember to always follow your doctor’s instructions when it comes to caring for your PD catheter. Daily inspections of your access site are essential in making sure you remain healthy and free from infection. If you think you may have contaminated your catheter, equipment or supplies, contact your dialysis care team. Remember that when it comes to peritonitis, the sooner you begin treatment, the better!
Sources:
(i) https://www.kidneyresearchuk.org/health-information/peritonitis
(ii) https://www.ncbi.nlm.nih.gov/books/NBK441979/
(iii) https://www.freseniuskidneycare.com/ckd-treatment/home-peritoneal-dialysis/about-peritonitis