If you’ve selected peritoneal dialysis (PD) as your mode of dialysis, there’s a lot to learn. Before you can begin PD, you’ll need to have a minor surgical procedure to place the PD catheter, a soft, flexible tube. Once your catheter is placed, your most important job is keeping it clean. Maintaining your catheter is especially vital if you’ve opted for PD. Read on to learn more about preventing PD catheter infections.
What Is Peritoneal Dialysis?
Most types of dialysis are performed by a medical team in a dialysis center, but PD is different. This type of dialysis can be performed in your own home or in any other clean, enclosed environment. i
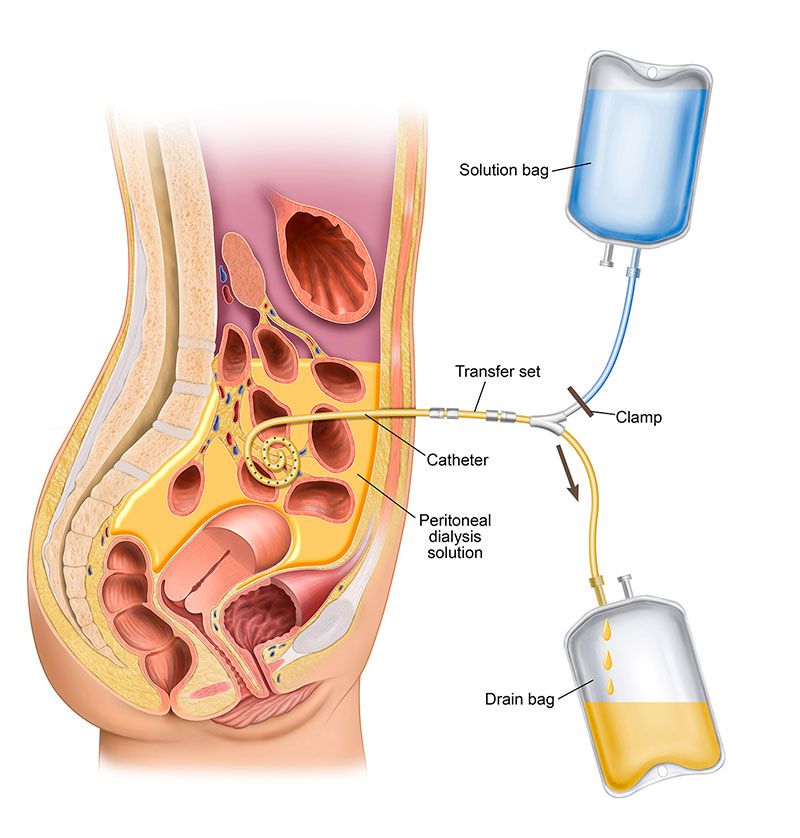
Peritoneal dialysis uses the lining of your abdomen to filter waste from your blood. The process gets its name from the lining of your abdomen, which is called the peritoneum. This lining is a membrane that surrounds the abdominal space called the peritoneal cavity.
When performing PD, using your catheter you will fill your peritoneal cavity (belly area) with dialysate and let it remain in your abdomen for a prescribed length of time. This is called dwell time. When the dwell time is over, you will drain the used dialysate from your abdomen through the PD catheter and refill your abdomen with fresh dialysate. This process of filling, dwelling and draining your abdomen is called an exchange. Each fill and dwell cycle usually takes between 30 and 40 minutes. The dwell time, typically 4 hours, is prescribed by your nephrologist. Depending on the type of PD you choose, you may do these exchanges manually or with the help of a machine.
PD treatments are done more frequently, so waste and toxins in your blood don’t have a chance to build up between treatments. Your doctor will tell you how many exchanges you should do each day. Most people do their PD exchanges at home, but you can do them any place that is well lit, clean and dry – at work, at home and while traveling.
What Is a PD Catheter?
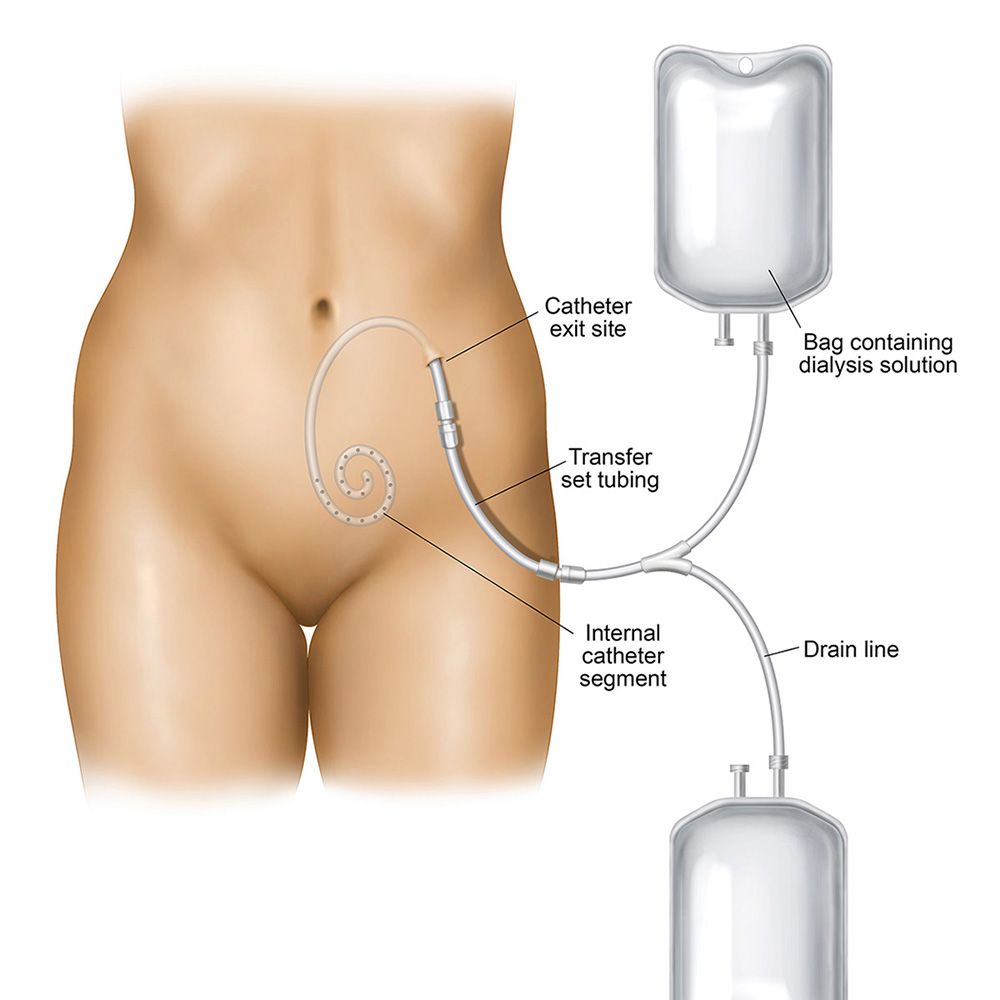
Before you can begin PD treatments, your vascular specialist will place a soft, flexible plastic tube called a catheter into your abdomen. The PD catheter allows dialysis fluid to enter your abdomen to clean your blood. The fluid then drains back out through the catheter and is discarded. i
PD patients are responsible for taking care of their dialysis access. Peritoneal dialysis only works when your PD catheter is functional. Problems with a catheter can interfere with your dialysis treatments. In some cases, catheter problems can even be life-threatening.
Your catheter is a critical piece of dialysis equipment. A well-functioning catheter allows you to continue receiving dialysis treatments on schedule, but a blocked or infected catheter can put your health at risk.
What Problems Can Affect My PD Catheter?
More than 84 percent of PD catheter problems are caused by an infection. ii Other PD complications include catheter obstruction, dislocation or leakage. iii
Most infections result from bacteria living on human skin. As long as these bacteria remain on the surface of the skin, they usually don’t cause any problems. When they enter the bloodstream through a cut, scrape or surgical incision, an infection can take hold.
All dialysis patients are at an increased risk of infection. That’s because end-stage renal disease (ESRD) weakens your immune system. PD patients are at increased risk of infection because the PD catheter is a direct connection between the outside world and your internal environment.
What Types of Infection Can Affect My Catheter?
Exit site infections affect the skin surrounding your catheter. iv These infections are especially common for people on PD. Many infections can be prevented through proper hygiene and the use of antibiotic ointment. Some exit site infections are virulent and can take hold even if you’re most careful about taking precautions.
Tunnel infections affect the pathway of the catheter inside the body. These infections can affect many layers of skin and tissue. Tunnel infections sometimes develop after PD catheter placement procedure. A tunnel infection must be treated right away, or it may turn into peritonitis. iv
Peritonitis is the most serious type of PD related infection. This infection affects the lining of your abdominal wall and can also spread to the organs inside your body. v If you develop peritonitis, you will need urgent medical care and most likely antibiotic therapy. In severe cases you may need to have surgery to remove and/or replace your catheter.
Catheter infections may seem like a mere inconvenience, but they can be life-threatening. That’s why it’s essential to keep your access area clean. It’s also vital that you report any signs of infection to a doctor right away.
What Are Some Symptoms of an Infected Catheter?
Symptoms of an infected catheter can include: vi
- Pus draining from the catheter exit site
- Red streaks around the access area
- Red, inflamed skin
- Swelling, warmth, or increased pain
- Fever
Examine your access area every day to check for signs of infection. If you notice any new or worsening symptoms, notify your PD care team immediately. Most infections can be easily treated, but early treatment is crucial.
What Treatments Can Help Resolve a PD Catheter Infection?
Most PD catheter infections are caused by bacteria. These infections are usually treated with antibiotics. Mild exit site infections often clear up with antibiotic ointment and careful hygiene.
Severe infections may need more intensive care. You may need to take oral antibiotics for up to six weeks. In some cases, oral antibiotics may fail to clear the infection. Some bacteria have become resistant to many common antibiotics. If you have an antibiotic-resistant infection, you may require IV antibiotics and/or catheter removal. vi
How Can I Avoid a PD Catheter Infection?
Good hygiene is your most valuable defense in the fight against infection. Wash your hands with hot, soapy water several times a day. Make sure to wash your hands before and after performing an exchange. If someone else helps you with your exchanges, make sure they wash their hands as well.
Most doctors recommend that people on PD shower daily, however you need to keep your catheter and the site dry. Your PD nurse will instruct you how to do this. You may need to avoid baths and swimming pools. If you aren’t able to shower every day, your doctor can help you develop a catheter care plan that meets your needs.
Your medical team can provide you with more advice on caring for your PD catheter. You’re nephrologist may prescribe to the use antibiotic ointment at your exit site. Use this as directed. Don’t skip doses or stop using the ointment without your doctor’s permission.
Here are some other general catheter tips: vii
- Whenever uncovering your PD catheter, be sure to wear a mask and gloves.
- Check your catheter exit site and surrounding area daily for signs of infection.
- Report any new symptoms to your doctor right away.
- Don’t pick any scabs or blemishes near your catheter.
- Avoid tight clothing or restrictive undergarments.
- Choose breathable clothing materials, like cotton.
- Try not to rub, scratch, or pull on the catheter.
- Keep your catheter covered with a sterile dressing and tape or secure your catheter to your skin.
Starting dialysis can be overwhelming. Your medical team will provide you advice and recommendations. Sometimes it can be tough to make sense of all this information but it’s important to follow your doctor’s advice at all times. Cooperating with medical recommendations can help you avoid infections and other complications.
Sources:
i. Mayo Clinic. (2018, March 22). Peritoneal dialysis. Retrieved February 20, 2019, from https://www.mayoclinic.org/tests-procedures/peritoneal-dialysis/about/pac-20384725
ii. Moist, L. M., & Al-Jaishi, A. A. (2013). The upfront risks of vascular access complications. Journal of the American Society of Nephrology, 24(10), 1509-1511. doi:10.1681/asn.2013070759
iii. Akoh JA. Peritoneal dialysis associated infections: An update on diagnosis and management. World J Nephrol. 2012;1(4):106-22.
iv. Fresenius Medical Care. (2016, July) Management of catheter infections. Retrieved February 20, 2019, from https://www.advancedrenaleducation.com/content/management-catheter-infections
v. Mayo Clinic. (2018, June 6). Peritonitis. Retrieved February 20, 2019, from https://www.mayoclinic.org/diseases-conditions/peritonitis/symptoms-causes/syc-20376247
vi. National Kidney Foundation. (2015). Hemodialysis catheters: How to keep yours working well. Retrieved February 20, 2019, from https://www.kidney.org/atoz/content/hemocatheter
vii. Berns, J. (2017, August 22). Patient education: Hemodialysis (Beyond the Basics). In Steve Schwab (Ed.), UpToDate. Retrieved February 20, 2019, from https://www.uptodate.com/contents/hemodialysis-beyond-the-basics