While both methods are currently used for dialysis, there are significant differences between a peritoneal dialysis (PD) catheter and a central venous catheter (CVC).
When your kidneys fail to function properly, your doctor may suggest and start planning for dialysis. During the planning process, it is important to understand the different types of dialysis treatment options available, as well as their advantages and disadvantages, in order to find the right treatment for your needs as well the one that will give you the best quality of life.
Let’s explore peritoneal dialysis catheters and central venous catheters in-depth, as these are two dialysis access options for dialysis that may be suggested by your doctor.
What are the different types of dialysis?
In order to fully understand the differences between a PD catheter and CVC, it’s essential to first understand the two different approaches to dialysis and how each one works.
There are two different types of dialysis: hemodialysis and peritoneal dialysis.
During hemodialysis, blood is pumped out of your body to a machine that incorporates a filter called a dialyzer (also known as an artificial kidney), with the assistance of the machine the dialyzer filters your blood of excess fluid and waste products and then returns the filtered blood to your body. This process is completed by connecting your vascular access to soft tubes that facilitate the blood flow to and from the dialysis system. Central venous catheters, as well as AV fistulas and grafts, are the primary types of hemodialysis access.
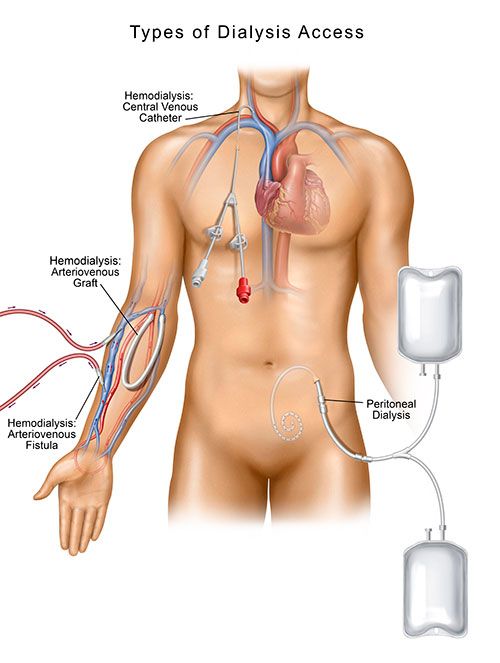
In peritoneal dialysis, instead of connecting to a dialyzer, the inner lining of your abdomen (your peritoneal membrane) acts as a natural filter. A soft tube, called a catheter, is placed in your abdomen by a vascular specialist. It is through this catheter that a sterile cleansing solution is instilled into your body. The solution is responsible for the filtering process, and once it is complete, the fluids are drained from your abdominal cavity through same catheter. (i, ii)
What are the differences between a PD catheter and CVC placement?
There are three different approaches to the insertion of a PD catheter: surgical, percutaneous, and laparoscopic.
Surgical PD Catheter Placement
A surgical approach to PD catheter placement is usually planned at least three weeks before your first exchange. During the procedure, you will receive either general or local anesthesia. A surgeon will make incisions around your belly button and then guide a catheter until it is placed in your belly, also known as your peritoneal cavity. Once secured in place, it will be covered by a sterile dressing over the point where the catheter was placed. As part of your dialysis training, you will learn how to clean and take care of this insertion site properly. (iii)
The PD catheter can be used as soon as it is placed, but patients may have better treatment outcomes if the body has a few weeks to heal from the surgery.
Percutaneous PD Catheter Placement
Your PD catheter can also be placed in an outpatient setting during a minimally invasive procedure. This approach is called percutaneous PD catheter placement and, as opposed to surgical insertion, is performed under only local anesthesia and sedation while utilizing an imaging technique called fluoroscopy.
Fluoroscopy is a type of medical imaging that shows a continuous X-ray image on a monitor, much like an X-ray movie, so your vascular specialist can view the inside of your abdomen while performing the procedure. The procedure begins by the vascular specialist first making a series of small punctures in your skin to access the inner lining of your abdomen (called the peritoneum). The PD catheter is then passed through a small tunnel in your belly into the peritoneum and secured in place. Catheters have small cuffs that keep it in place. After the PD catheter has been inserted, your vascular specialist will place sutures around the catheter on the outside of your abdomen and cover the site with a sterile dressing. You will be instructed to keep the area clean by your vascular specialists, similar to how you would with surgical placement.
Percutaneous catheters can be used for dialysis exchanges within 24 hours, which makes it an extremely effective method if dialysis needs to be started urgently (vi).
Laparoscopic PD catheter placement
In general, laparoscopy is a minimally invasive type of surgery, which is performed by making small incisions into the belly and utilizes a camera for visualizing surrounding tissues or organs. A vascular specialist performs laparoscopic PD catheter placement by first making three small incisions around your belly button. The first incision is for insertion of the small camera. The second incision is for the introduction of the catheter which will be passed underneath the skin and the final incision is for the exit of the catheter, i.e. the part of the catheter that remains outside of your body. Once the catheter is tunneled to its appropriate location under guidance of the camera, a suture is tied to secure it in place.
Laparoscopic placement offers a faster recovery time and minimal incisions compared to open surgery and, like percutaneous placement, dialysis can be started urgently if needed (vi).If you are going to receive peritoneal dialysis through a peritoneal catheter, you will first require a procedure to place the catheter in your belly. This is usually planned at least three weeks before your first peritoneal dialysis treatment. A PD catheter can be used as soon as it is placed, but patients may have better treatment outcomes if the body has a few weeks to heal after insertion. During the percutaneous procedure, you will receive local anesthesia. A surgeon will make a small cut near your belly button and then guide a catheter until it is placed into your peritoneal space, also known as your peritoneal cavity. Once secured in place, it will be covered by a sterile dressing over the point where the catheter was inserted. As part of your dialysis training, you will learn how to clean and take care of this insertion site properly. (iii)
CVC Placement
With a CVC, a y-shaped catheter is placed by puncturing the internal jugular vein in the neck (most often on the right side), and the catheter is then advanced downwards toward the chest. The internal tip resting directly in the upper right chamber of your heart. The catheter used during dialysis is referred to as a tunneled catheter because it is placed under the skin. Your physician numbs the area of skin for insertion and may use imaging to guide the catheter into its correct location. After it’s inserted, two soft tubes will be visible on the outside of your body in the upper chest area. These tubes connect to the dialysis machine during treatment. One tube is used to draw blood from your vein out of your body and into the dialyzer to be filtered. The other tube allows cleaned blood to be returned to your body. A CVC can be used immediately if needed. (iv)
What are the differences between a PD catheter and CVC when dialyzing?
The main difference between a PD catheter and CVC when dialyzing is how the blood is filtered.
With PD, no machine is used for dialysis. As mentioned before, the lining of your belly acts as the “filter” for cleaning the blood. During PD treatment, a dialysis solution comprised of water, salt and other additives will flow from a bag through the catheter and into your belly. Once the bag is empty, you can disconnect it and place the cap on your catheter and go about your normal activities. While the solution remains in your belly, it absorbs wastes and extra fluid from your body.
After a prescribed amount of time typically 4-6 hours, the solution is drained out of your body, and you repeat the process of refilling your belly with fresh solution. This process is called an exchange, and each exchange(minus the prescribed dwell time) takes about 30 to 40 minutes. A person will typically complete this exchange four to six times a day. All of these exchanges happen at home/work, i.e., you do not go to a dialysis center for treatment.
When receiving hemodialysis with a CVC, the soft tubes of your access are connected to a hemodialysis machine. One tube is responsible for removing blood from your body into the machine to be filtered, while the other tube returns clean blood to your body. This typically occurs three days a week and can last approximately 4 hours at a time. This type of dialysis treatment is completed in an outpatient dialysis center unless you have decided on home dialysis treatment.
What are the Advantages and Disadvantages of a PD catheter?
Advantages of a PD Catheter:
- Increased quality of life: Because PD is completed at home, you can continue to live a relatively normal life without being hindered by having to go to a dialysis center. Some types of dialysis exchanges can even be completed at nighttime when you are sleeping, so it doesn’t interrupt your daily routine.
- Less restricted diet: Because peritoneal dialysis occurs more continuously than hemodialysis, it results in less of an accumulation of wastes, sodium, and fluid so you can enjoy a more flexible diet than you would on hemodialysis.
- Longer lasting residual kidney function: In comparison to people who use hemodialysis, people who use peritoneal dialysis might retain kidney function slightly longer. PD may also put less strain on your heart and other blood vessels because it is a more continuous type of dialysis since exchanges happen every day.
- No needles: There are certain types of hemodialysis (AV fistula and AV grafts) that require the insertion of large needles to complete dialysis. No needle placement is required for peritoneal dialysis. (i, iv)
Disadvantages of a PD Catheter
- Risk of infection: Bacteria can enter your body and cause infection through the catheter when you connect and disconnect your bags. Your dialysis team will educate you on the best practices when it comes to taking care of your insertion site as well as your equipment. Should you develop a fever, nausea and vomiting or any signs of warmth, redness or pain at the site, you should contact your doctor immediately.
- Hernia: Holding fluid in your abdomen for long periods may strain your abdominal muscles and can result in an increased chance of developing a hernia.
What are the Advantages and Disadvantages of a CV Catheter?
Advantages of a CVC:
- Immediate access: A CVC can be used as soon as it is placed, so it is a good choice if urgent or emergent dialysis is needed.
- No needles: Like PD, no needles are required for dialysis treatment with a CVC. During dialysis with a CVC, the tubes from the catheter connect directly to the tubes on the dialysis machine, negating the need for needles.
Disadvantages of a CVC:
- Serious infection from CVC: Infections can be localized (to the area of the insertion site) or systemic. Infection is responsible for the removal of about 30%–60% of CVCs and hospitalization rates are higher in CVC patients than patients with other types of dialysis accesses. The most dangerous infectious complication is catheter-related bloodstream infection (CRBSI), associated with high rates of morbidity and mortality. (v)
- Risk of Clots: Blood clots can form on and/or in the internal opening of the catheter and slow or entirely block the blood flow. When this occurs, it can cause difficulty in dialyzing, and it must be tended to in order to have an adequate blood flow rate for dialysis.
- Damage to Blood Vessels: Over time, a CVC can cause a stenosis, or narrowing, of the vein(s) where it is placed. This can cause damage to the walls of the vein and may prevent blood from flowing adequately.
Is a Peritoneal Dialysis Catheter or CVC right for me?
When making a decision about the type of treatment to have, you should take into consideration the advantages and disadvantages of each dialysis option as well considering the quality of life each treatment type offers.
While a CVC may be necessary if you need dialysis urgently, you should talk to your doctor about long-term options for receiving dialysis. Peritoneal dialysis is an effective form of dialysis and generally has better long-term benefits and advantages. With peritoneal dialysis, you can control extra fluid more easily, and this may reduce stress on the heart and blood vessels. Your diet is also more flexible, and you can do more of your daily activities, which can provide for a better quality of life.
If you are ready to talk to a specialist at Azura Vascular Care about your access treatment options, you can contact us at 866.996.9729 or find a center near you.
Sources:
(i) National Kidney Foundation. (n.d.). Peritoneal Dialysis: What You Need to Know. Retrieved August 1, 2019 from https://www.kidney.org/atoz/content/peritoneal.
(ii) National Kidney Foundation. (n.d). Hemodialysis Catheters: How to Keep Yours Working Well. Retrieved August 1, 2019 from https://www.kidney.org/atoz/content/hemocatheter
(iii) National Institute of Diabetes and Digestive and Kidney Diseases. (January 2018) Peritoneal Dialysis. Retrieved August 1, 2019 from https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/peritoneal-dialysis
(iv) Mayo Clinic. (April 2019) Peritoneal Dialysis. Retrieved August 1, 2019 https://www.mayoclinic.org/tests-procedures/peritoneal-dialysis/about/pac-20384725
(v) Santoro, D., Benedetto, F., Mondello, P., Pipitò, N., Barillà, D., Spinelli, F., … Buemi, M. (2014). Vascular access for hemodialysis: current perspectives. International journal of nephrology and renovascular disease, 7, 281–294. doi:10.2147/IJNRD.S46643