The population of those aged 65 years or older with end-stage renal disease (ESRD) continues to grow rapidly in the United States. If the decision is to start hemodialysis (HD) as the most suitable modality, planning for the appropriate vascular access requires careful consideration of several factors.
Arteriovenous fistulas (AVFs) have long been considered the gold standard and recommended by many national clinical guidelines as the vascular access of choice in HD patients. Are they the best option for patients over the age of 65? Read on to learn more.
What Are My Options for Vascular Access?
If you need to begin hemodialysis, you must first have an access created. A dialysis access allows your blood to flow from your body to the dialysis machine for cleaning, and then back to your body. The access is usually placed in your arm or leg. There are three different types of hemodialysis access options.
A central venous catheter is a thin, Y-shaped plastic tube. A vascular specialist inserts the catheter into a vein in your chest, neck, or groin. A catheter is often used as a temporary access. Other types of access, such as grafts or fistulas, are considered better long-term options. A catheter isn’t as reliable as a graft or fistula. It’s also more prone to infection and clotting, but it allows you to start dialysis right away if your situation is urgent. [i]
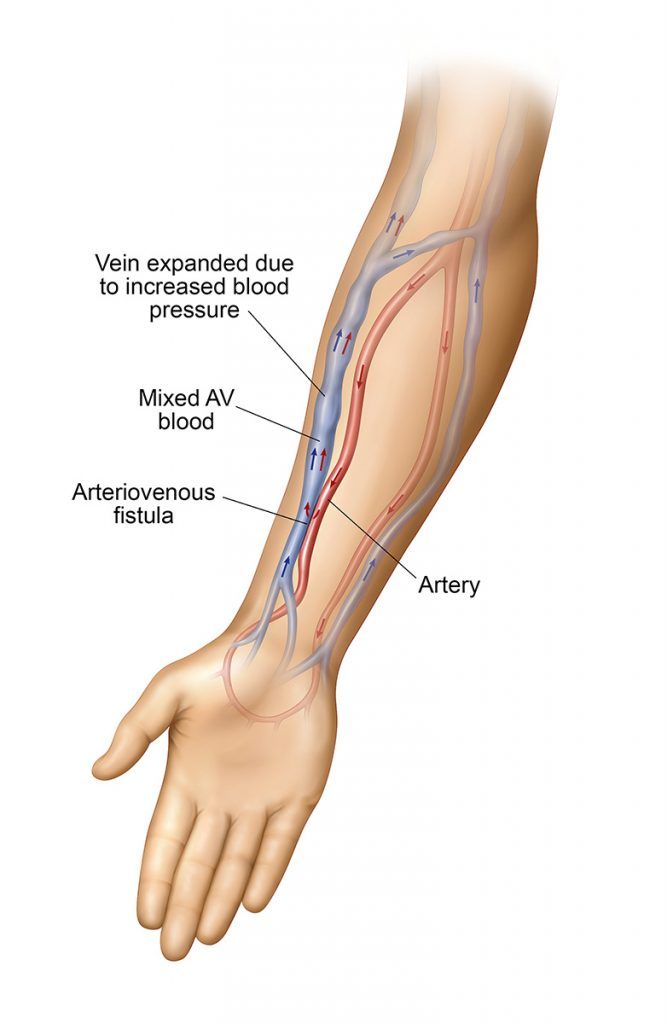
An AV fistula is generally considered the best option for dialysis access. During fistula creation, your vascular specialist makes a direct connection between a vein and an artery. A properly-created fistula allows plenty of blood to flow from the body to the artificial kidney and the dialysis machine. Fistulas can last for many years. Once created a fistula can take weeks or months to mature. If you need to start dialysis immediately, you might need a catheter temporarily while you wait for your fistula to mature. [i]
An AV graft is a biocompatible synthetic tube which is used to connect a vein to an artery. Like a like a fistula it provides a sufficient blood flow rate from the body to and from the hemodialysis system. Unlike a fistula, which uses the native veins and arteries the AV graft is an artificial conduit used to form the connection between a vein and an artery. Grafts aren’t quite as durable as fistulas. They’re also more likely than fistulas to become clotted, but they may be ready for use more quickly than a fistula. A graft is often ready for use within just a few weeks. A graft can be a better option for people with small or insufficient veins. [i]
Your care team can help you select the access that’s best for you. It’s important to remember that each person on dialysis has unique medical needs. Although fistulas are the best option for many people, a different type of access may be recommended. If your care team recommends a catheter or a graft, make sure you understand the reasons behind this
Is an AV Fistula the Best Choice for Me?
Although fistulas are the preferred option for most dialysis patients, for many patients it can be difficult for their fistula to mature and function adequately. Fistulas can have a high early failure rate, especially for patients over age 65. [ii] Sometimes a vascular specialist must attempt a fistula creation procedure more than once. If your fistula fails to mature and function properly, you may need a different type of access.
Your nephrologist can help you determine which kind of access will best meet your individual needs. An experienced vascular specialist can also help you learn how to minimize the risk of fistula failures. Some fistula failures can’t be avoided but choosing the right vascular specialist can help boost your fistula’s chances for success.
What Are Some Health Risks That Dialysis Patients May Face?
Infection is a risk for people living with end-stage renal disease (ESRD). ESRD compromises your immune system, so you’re more susceptible to infections. Access surgery can create an added opportunity for bacterial infections.
Some patients develop AV fistula infections after their surgery. Others develop infections further down the line. No matter when infections occur, they have the potential to be life-threatening. Older dialysis patients are at an increased risk of infection due to the normal aging process and its effect on the immune system.
Studies have suggested that AV fistulas offer the lowest risk of infection and hospitalization. Severe infections can land you in the hospital and may lead to problems with breathing or circulation. A recent study concluded that fistulas offer dialysis patients a lower risk of these complications. That translates to better overall survival rates. [ii]
How Can I Make Sure My Fistula Procedure Is a Success?
Before you undergo an access procedure, ask your vascular specialist about their experience and qualifications. A skilled vascular specialist can provide you with better post-fistula creation outcomes. Your physicians will work with you as you make decisions about all your options for dialysis.
If you and your access care team decide that you’re a good candidate for a fistula, you’re off to a great start. Fistulas are durable and less prone to clotting or infection. A successful fistula will provide a blood flow rate sufficient to ensure the delivery of an adequate hemodialysis treatment. Most vascular specialists agree that they’re the preferred access option for most dialysis patients. [ii]
Fortunately, the right surgical techniques can maximize your chances of success. Several studies have shown that the surgeon’s skill plays a tremendous role in your surgical outcome. One study revealed that the fistula’s failure rate was 34 percent lower when performed by an experienced surgeon. [ii]
Pre-Surgical Tests
Preoperative vascular mapping is an essential part of your fistula creation procedure. A skilled specialist doesn’t stop with a basic physical examination. Instead, he or she uses imaging tests such as an ultrasound to identify the best vessels for fistula creation. One study suggested that using ultrasound mapping doubled a patient’s chances for successful fistula placement. [ii]
New AV Fistula Creation Technology
New technology may help increase your fistula’s chances of success. One promising new method is a minimally-invasive, intravascular percutaneous procedure for fistula creation. [ii] Percutaneous procedures use needle punctures and catheters to connect an artery and vein rather than a scalpel.
Because the procedure is less invasive than surgery, there’s a lower risk for complications. Percutaneous procedures offer a much lower risk for infection. Since infection is a constant concern for patients with ESRD, this is a real advantage.
When used alongside ultrasound technology, these percutaneous techniques also offer greater precision. A more precise procedure can translate to much higher success rates. Rather than general anesthesia, these procedures use only local anesthetic and/or conscious sedation.
This can be a significant advantage for patients over age 65 because they are more likely to have chronic diseases than younger patients. If you are placed under general anesthesia, you may need to stay in the hospital overnight. Long hospital stays can sometimes lead to additional complications, like hospital-acquired infections. General anesthesia can also sometimes trigger breathing problems in older patients. Avoiding general anesthesia may reduce your chances of developing life-threatening complications after surgery. [ii]
Fistula Location
Recent studies have suggested that the location of a fistula plays a vital role in the procedure’s outcome. Compared to younger patients, those over age 65 have a higher fistula failure rate if their fistula is placed in the lower arm than if it is placed at the elbow or in the upper arm. [ii] Vessels in the upper arm are of adequate size and less affected by atherosclerosis, or the buildup of plaque on the inner walls of . [iii]
It’s important to recognize that fistulas are still the preferred access option for most dialysis patients. The elderly have specific health care requirements and because they offer a lower risk for infection, fistulas can be beneficial for patients over age 65 but it’s dependent on various factors including having an experienced vascular specialist to perform your procedure.
Your vascular specialist will work with you and your care team to select the best dialysis vascular access for you. After you undergo your access creation procedure, your care team will continue to provide support as you make decisions about your dialysis treatments. Starting dialysis means that you will need to make many different choices. Having a care team you can trust will make these decisions easier.
To learn more about your access options, download our free information sheet, Understanding Your Dialysis Access. Then call 866.996.9729 to schedule an appointment with a vascular specialist today.
Sources:
(i.) National Kidney Foundation. (2015). Hemodialysis access. Retrieved February 20, 2019, from https://www.kidney.org/atoz/content/hemoaccess
(ii.) Asif, A., Bakr, M., Levitt, M., & Vachharajani, T. (2018). Best vascular access in the elderly: Time for innovation? Blood Purification, doi:10.1159/000494591.
(iii.) Palmes, Daniel, Kebschull, Linus, Schaefer, Roland M., Pelster, Friedrich , Konner, Klaus; Perforating vein fistula is superior to forearm fistula in elderly haemodialysis patients with diabetes and arterial hypertension, Nephrology Dialysis Transplantation, Volume 26, Issue 10, 1 October 2011, Pages 3309–3314, https://academic.oup.com/ndt/article-lookup/doi/10.1093/ndt/gfr004