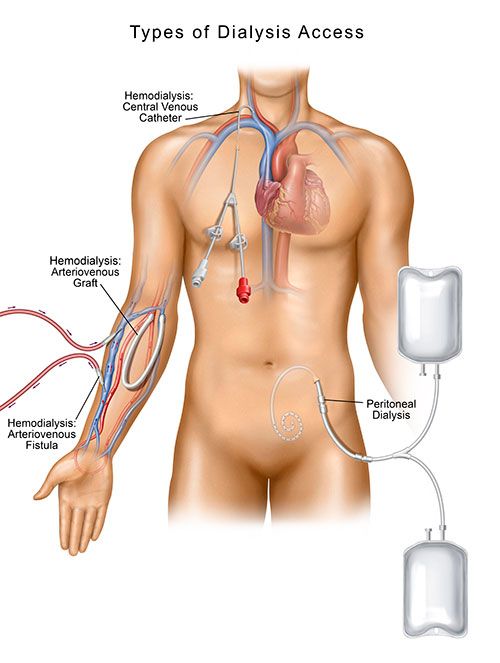
For patients living with end-stage renal disease (ESRD), dialysis access management is extremely important. Many ESRD patients require hemodialysis (HD) treatments – a process in which blood is transported from your body for cleaning. A vascular access is created so that blood can be drawn from the body and run through a dialysis machine, where excess fluid and toxins are removed from the blood. (i) The filtered blood then flows back through the access into the body.
Another type of dialysis, called peritoneal dialysis (PD), uses the abdominal lining and a specialized sterile solution to clean the blood inside your body. Before you can receive peritoneal dialysis, an access called a peritoneal dialysis catheter (PD catheter) must be placed.
The dialysis access is essentially a dialysis patient’s lifeline to treatment and good health and having a well-functioning access that handles adequate blood flow allows for the most effective dialysis treatment.
But what happens when your access becomes dysfunctional? Read on to learn about the importance of dialysis access management.
Access Creation
Dialysis starts with access creation. For patients who need hemodialysis, an access into the bloodstream must be established. A central venous catheter (CVC), an arteriovenous fistula (AV fistula) or an arteriovenous graft (AV graft) are the three most common types of accesses used for hemodialysis. Peritoneal dialysis requires a different type of access known as a peritoneal dialysis catheter (PD catheter).
A vascular specialist—an interventional radiologist, interventional nephrologist or vascular surgeon—will work closely with the patient and their nephrologist to determine the type of access that is best for the patient, and will also be the clinician to provide the care and maintenance of that access.
Access Dysfunction
When your access isn’t performing optimally during dialysis, you may need to see a vascular specialist for dialysis access management so that you may continue with your dialysis treatments. Access interventions, including a fistulogram, angioplasty, stent placement, thrombolysis and/or thrombectomy, may be performed to improve or restore your access’s blood flow.
Fistulogram
If an AV graft or AV fistula is not functioning well during hemodialysis, a fistulogram may be performed. During this minimally invasive x-ray procedure, IV contrast is used to view the access and identify areas where the blood vessel is too narrow (stenosis), abnormally enlarged (pseudoaneurysm), or partially or completely blocked (clotted).
A fistulogram is a commonly performed procedure, lasting less than one hour on average. A small tube (catheter) is inserted into the graft or fistula and the contrast (dye) is injected as radiographic images (fistulogram) are taken. Typically, patients are asked not to eat for six hours prior to the procedure. If needed, conscious sedation is available to manage pain and anxiety.
Angioplasty
If abnormal narrowing (stenosis) is seen during the fistulogram, further dialysis access management is needed. An AV graft or fistula may be treated with angioplasty, a minimally invasive procedure used to widen a narrowed portion of the fistula or graft to restore the blood flow to the desired rate.
Using imaging guidance, a catheter with an inflatable balloon mounted to it is inserted through the skin into the fistula or graft and advanced to the location of the narrowing or blockage. After correct placement has been determined, the balloon is inflated and deflated, expanding the vessel wall to increase blood flow through the access; once adequate blood flow through the vessel has been restored, the balloon catheter is deflated and removed.
During angioplasty, you may feel slight pressure when the catheter is inserted, but there should be no serious discomfort. As the contrast material passes through your body, you may experience a warm feeling, which should subside quickly. After the procedure, your access site will be checked for bleeding or swelling, and your blood pressure and heart rate will be monitored. Although angioplasty is an effective way to manage a dialysis access, sometimes stent placement is needed to keep the vessel from re-narrowing. This also helps to maintain adequate blood flow through the access.
Stent Placement
Stent placement, another minimally invasive dialysis access management procedure, is sometimes performed in conjunction with angioplasty. A stent is a small, wire mesh tube that expands to hold the affected segment of the blood vessel open if angioplasty alone isn’t successful, and then remains in place after the procedure, allowing for improved blood flow.
Thrombolysis and Thrombectomy
A declot procedure is a common dialysis access management procedure performed when a fistula or graft is partially or entirely clotted. Various techniques may be used to remove the clot from the access area in order to re-establish adequate blood flow.
In the case of a clot in your access, an angioplasty balloon may be inserted to open the clotted or blocked area(s) in the vein. Then, the clot can be dissolved with medication or removed or broken up with a specialized mechanical device.
The vascular specialist will determine whether the clot can be best treated by thrombolysis (a clot-dissolving medication), by thrombectomy (breaking up and removing the clot) or by mechanical thrombectomy (using a mechanical medical device), or a combination of methods. These techniques are relatively quick procedures and can be performed safely in an ambulatory surgery center or comparable high-quality outpatient setting.
Using fluoroscopic imaging (a type or x-ray) and contrast dye to help view and define the blood vessel, your vascular specialist will insert a catheter through the skin into an artery or vein and direct it to the thrombosis, or clot. The blood clot will then be treated in one of two ways:
- Thrombolysis: A catheter is used to instill a clot-dissolving medication into a blood clot in a fistula or graft. Once the clot is dissolved, the catheter is removed.
- Thrombectomy: A catheter and/or a mechanical device is used to break up and remove the clot.
At the end of these procedures, direct pressure will be applied at the access site to stop any bleeding. The opening in the skin will be covered with a simple dressing; typically, no sutures are required. When you return home, you should relax for the rest of the day. You’ll be able to eat and drink as usual and return to your usual activities 24 hours after your procedure.
Dialysis access management starts with access creation and continues with interventions that keep them fully functional. Understanding the importance of dialysis access management will allow you to properly care for your access and recognize abnormalities so you can continue to receive the dialysis treatments you need. Remember, your dialysis treatments will be most successful if your access is functioning well. For tips on dialysis access care and management, view Dialysis Access Care & Management.
Sources:
(i) Fresenius Kidney Care. (n.d.). What Is Dialysis? Retrieved December 13, 2018, from https://www.freseniuskidneycare.com/ckd-treatment/what-is-dialysis.