If the kidneys no longer work effectively, dialysis can replace some of the functions of the kidney by eliminating waste and unwanted fluid from the blood. For hemodialysis, a vascular access is needed to get to the blood. There are three types of hemodialysis vascular access: fistula, graft and catheter. All three of these can act as a hemodialysis lifeline because the access allows blood to reach the dialysis machine, where it is cleaned, then the filtered blood is returned to the body. Your blood is filtered at about one quart per minute during dialysis. (i) But when your access isn’t performing optimally, you may need to see a vascular specialist for dialysis access care and management. Access intervention, including angioplasty, stenting, thrombectomy and thrombolysis, may be performed to improve or restore your access’s flow. Read on for more information about these dialysis access management procedures.
Angioplasty
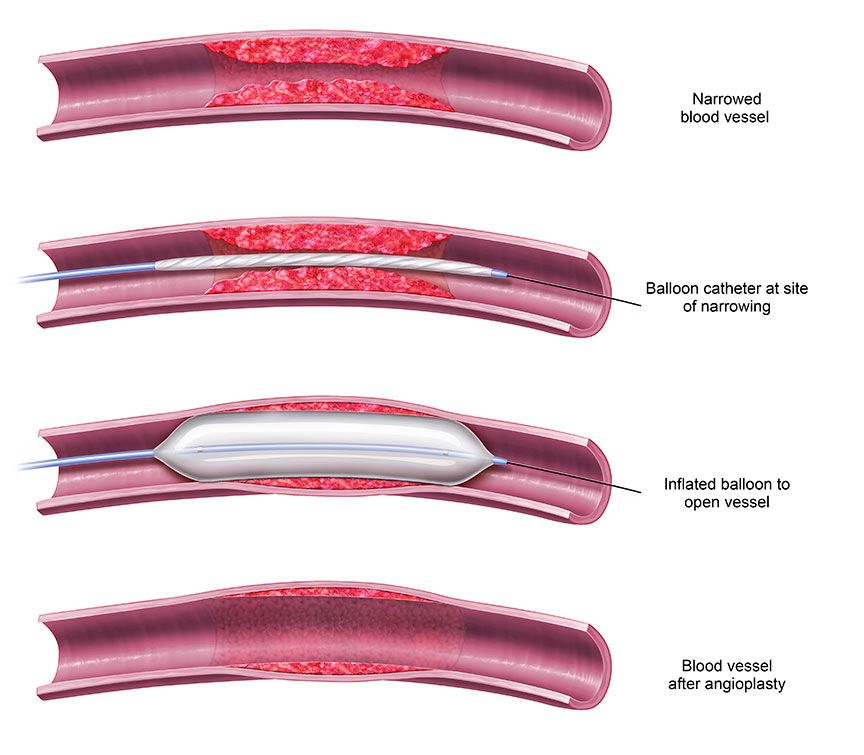
If a fistula doesn’t develop, or if it narrows—called stenosis—or forms clots—called thrombosis—angioplasty may be required. Angioplasty is a minimally invasive procedure used to widen a narrowed fistula or graft to restore the necessary blood flow. It is usually performed on an outpatient basis using local anesthesia to numb the incision area. Usually conscious sedation is used to manage pain and anxiety.
Using imaging guidance, an inflatable balloon mounted to the tip of a catheter is inserted through the skin into the fistula or graft and advanced to the location of the narrowing or blockage. There, the balloon is inflated and deflated, expanding the vein or artery wall to increase blood flow through the access; once the vessel is enlarged by the balloon it is deflated prior to removal. In the case of a clot, the balloon is inserted to open up the clotted or blocked area(s) in the vein. Then, the clot can be dissolved with medication or removed or broken up with a specialized mechanical device.
During the procedure, you might feel slight pressure when the catheter is inserted, but no serious discomfort. As the contrast material (used to visualize the interior of the access vessels) passes through your body, you may experience a warm feeling, which should ease quickly. After the procedure, the exterior of your access site will be checked for bleeding or swelling and your blood pressure and heart rate will be monitored.
Although angioplasty is an effective way to manage a dialysis access, it may need to be repeated periodically to keep the access continually functioning well.
Stenting
Stenting is also a minimally invasive procedure that is performed in conjunction with a balloon angioplasty procedure. A stent is a small wire mesh tube that expands to hold the affected blood vessel open if angioplasty alone isn’t successful, and then remains in place after the procedure, allowing for improved blood flow.
This, too, can safely and effectively be performed as an outpatient procedure.
Thrombectomy and Thrombolysis
Your doctor will determine whether the clot will be best treated by a clot-dissolving medication (thrombolysis), by breaking it up and removing the clot (thrombectomy) or by using a mechanical device (mechanical thrombectomy), or a combination of methods. Both are relatively quick procedures that are usually completed in less than one hour and can be performed safely in an ambulatory surgery center or comparable high-quality outpatient setting.
Using X-ray images to see and contrast dye to help define the blood vessel, your vascular specialist will insert a catheter through the skin into an artery or vein and direct it to the thrombosis, or blockage. The blood clot will then be dissolved in one of two ways:
- Thrombectomy, where a thin tube called a catheter, and/or a mechanical device is used to mash up and remove the clot.
- Thrombolysis, where a catheter is used to instill a clot dissolving medication into a blood clot in a fistula or graft to dissolve it. Once the clot is dissolved the medication is pulled back into the catheter to be removed.
At the end of these procedures, after the clot and the catheter are removed direct pressure will be applied at the access site to stop any bleeding. The opening in the skin will be covered with a dressing; typically, no sutures are required.
For more information about dialysis access care, download Understanding Your Hemodialysis Access or call 866-996-9729 to schedule an appointment with a vascular specialist.
Sources:
(i) Penn Medicine. (n.d.). Hemodialysis access management. Retrieved September 24, 2018, from https://www.pennmedicine.org/for-patients-and-visitors/find-a-program-or-service/interventional-radiology/procedures-and-services/hemodialysis-access
(ii) Radiological Society of North America. (2017, January 23). Dialysis and fistula/graft declotting and interventions. Retrieved September 24, 2018, from https://www.radiologyinfo.org/en/info.cfm?pg=dialysisfistulagraft