Millions of Americans suffer from vein disease and many ignore the warning signs—only seeking vein disease treatment when venous leg ulcers or other complications arise. Vascular health is crucial to your well-being, and at Azura Vascular Care, we want you to be well-versed in vein disease and recognize the first signs of trouble.
Vein disease affects each person differently. We know from experience that it is always better to seek vein disease treatment sooner rather than later. If left untreated, vein disease will worsen over time.
Let’s look at the stages of vein disease, the signs and the symptoms and discover what you can do to reduce your risks and when you should take action.
The Early Stages of Vein Disease
Like many conditions, vein disease comes in stages. At first, you may not notice the signs and symptoms, but if you are at risk for vein disease—which we will discuss shortly—it is important to assess yourself. Start by looking for subtle changes in your legs.
In the early stages of vein disease, you may notice:
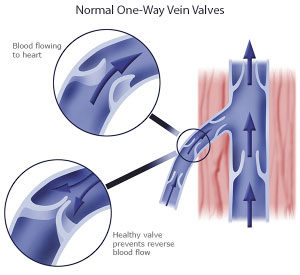
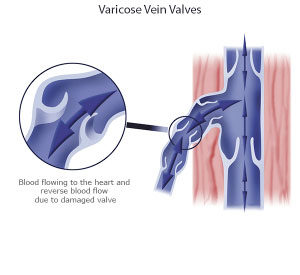
- Spider veins — These small, web-like veins or thin blood vessels are located near the surface of your skin. Spider veins look like scattered or tangled clusters of wispy red or purplish lines. Spider veins are flat. In other words, when running your hand over these veins, you will not feel bulging or swelling.
- Varicose veins — Unlike spider veins, varicose veins become bulging and ropy. People generally first notice their vein disease after the appearance of varicose veins. Not only are varicose veins unsightly, but they are often painful. Many people seek medical intervention when varicose veins contribute to leg pain, itching, tingling, swelling, restlessness, and a general heaviness in the legs.
The Later Stages of Vein Disease
In some cases, people with vein disease delay seeking treatment. However, the later stages of vein disease can significantly impair life quality. In the later stages, you may find it more difficult to relieve symptoms using over-the-counter medications or resting your legs.
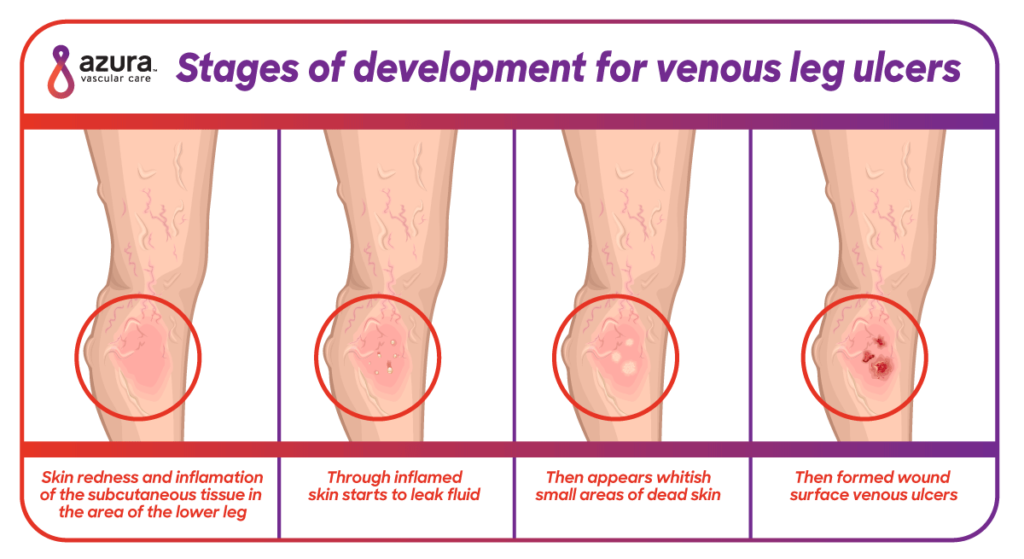
- Skin changes and swelling—Painful varicose veins can lead to leg swelling and skin discoloration. When leg veins are not working properly, the body is unable to absorb fluid and your legs will often swell. The pooling of bodily fluids can also change the skin color on your legs, often in the ankle area. Your skin may appear red or pale. At this stage in vein disease, it is easier to develop open sores—sores that take time to heal or sores that recur.
- Venous leg ulcers—These ulcers often follow leg swelling and skin discoloration. At this point, there is inadequate blood flow in the veins to provide nutrients to the skin to aid in healing. The injured skin heals very slowly or not at all. Venous leg ulcers may become chronic, painful, and debilitating, and since they are open wounds, they can also introduce bacteria into your legs, causing further pain and increasing the odds of infection.
Left untreated, vein disease may significantly damage your lymphatic system. When your lymphatic system does not work properly, it can lead to lipid accumulation and further damage to the walls of your veins. (1)
At Azura Vascular Care, we specialize in the treatment of even the most complex vein disease. Yes, it is always better to seek treatment for vein disease sooner rather than later, but it’s never too late to bring vein disease in line.
Vein Disease Risk Factors
There are many risk factors for vein disease, but the most common—especially in vein disease that begins with spider veins and varicose veins in the legs—include:
- Being 50 years of age or older
- Pregnancy
- Being overweight
- Prolonged sitting
- Prolonged standing
- Smoking
- Family history
A recent study out of Stanford Medical School found that height—being taller than average—may also increase your risk for developing painful varicose veins. The same study also found 30 genes that may be associated with varicose veins. (2)
If you are at risk, assess yourself. Do your legs feel heavy while standing, but better when resting? Do you notice spider veins forming? If you do notice these things, see a vascular specialist. If you do not have any of the warning signs, but you identify with the risk factors, take time out to exercise, avoid excessive sitting and standing, eat a healthy diet and stop smoking.
Vein Disease Treatment
When you take action against vein disease and seek vein disease treatment, you are doing more than preventing venous leg ulcers and painful varicose veins; you are taking a proactive step toward a healthy vein and lymphatic system.
Vein disease treatment—depending on the stage of vein disease—may include:
- Compression stockings — These snug-fitting stockings support your legs and help keep blood flowing properly through veins weakened by vein disease.
- Medications — Sometimes medications are prescribed, topically and orally, to fight infection or inflammation.
- Sclerotherapy — Injections into problematic veins reroute blood flow to healthier veins. Over time, the body reabsorbs the problematic vein or veins.
- Microphlebectomy — The problematic vein is removed through a small nick in the skin that does not require any stitches.
- Endovenous Thermal Ablation — High-frequency radio waves or heat via laser are used to shut down the problematic vein, which is reabsorbed by the body.
Take Action Against Vein Disease
The best time to take action against vein disease or seek treatment for vein disease is when you first notice the symptoms. However, it is never too late to restore your quality of life through vein disease treatments.
Contact Azura Vascular Care today at 844-832-VEIN (8346) to request an appointment with one of our vascular specialists. It is never too late to start feeling better!
Sources:
(1) Tanaka, H., Yamamoto, N., Suzuki, M., Mano, Y., Sano, M., Zaima, N., …. Unno, N. et al. (2016). Insufficient lymph drainage causes abnormal lipid accumulation and vein wall degeneration. Annals of Vascular Disease,9(4): 277-284. https://www.jstage.jst.go.jp/article/avd/9/4/9_oa.16-00122/_article/-char/en.
(2) White, T. Height may be risk factor for varicose veins. Stanford Medicine News Center. September 24, 2018. http://med.stanford.edu/news/all-news/2018/09/height-may-be-risk-factor-for-varicose-veins.html.