September is PAD Awareness month. The goal of Peripheral Artery Disease Awareness Month is to increase the public’s awareness about the risks of PAD as well as its relationships with other vascular diseases. PAD is the least recognized existing artery problem because many people mistake their symptoms as simply part of the aging process or being out of shape.[1] However, timely detection and treatment of PAD can significantly decrease the patient’s pain, discomfort, risk of heart attack and stroke, while also improving overall quality of life.
Understanding PAD
So, what is peripheral artery disease?
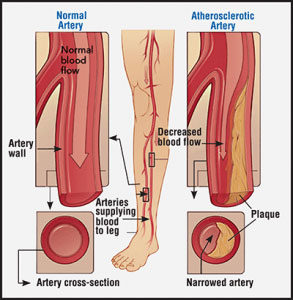 PAD is a serious medical condition that affects 8 to 12 million people in the United States.[1] It occurs when there is a buildup of extra cholesterol and plaque in the arteries (typically in the leg), which results in reduced or blocked blood flow to the legs and feet. PAD can cause severe health problems that can interfere with quality of life.
PAD is a serious medical condition that affects 8 to 12 million people in the United States.[1] It occurs when there is a buildup of extra cholesterol and plaque in the arteries (typically in the leg), which results in reduced or blocked blood flow to the legs and feet. PAD can cause severe health problems that can interfere with quality of life.
Find Out if You Are at Risk for PAD
There are various factors that could put you at risk for PAD. Your risk increases if you:
- Smoke or are a former smoker – The risk of developing PAD is up to four times higher for those who smoke or have a history of smoking.[1]
- Are over the age of 50 – One in every 20 Americans over the age of 50 has PAD[1]
- Suffer from Chronic Kidney Disease
- Have high blood pressure
- Have diabetes – One in every three people over the age of 50 with diabetes is likely to have PAD
- Have high cholesterol
- Have a family history – If your father has or had PAD, another vascular disease, or a heart attack or stroke, you have an increased risk of developing peripheral arterial disease.
- Are African American – African Americans have a 2.4 times greater chance of having a major amputation when compared with Caucasians.
If one or more of these PAD risk factors are present, you should ask your doctor about peripheral artery disease and take the PAD Risk Assessment.
RELATED: Understanding What Causes PAD
Signs and Symptoms
 PAD often remains undiagnosed because many people do not report their symptoms to their doctor’s.[1] If you experience any of the following symptoms you should talk to your doctor to determine if they are associated with PAD:
PAD often remains undiagnosed because many people do not report their symptoms to their doctor’s.[1] If you experience any of the following symptoms you should talk to your doctor to determine if they are associated with PAD:
- Non-healing wounds on feet or toes
- Foot ulcers or sores
- Lower temperature in one leg
- Poor nail growth and decreased hair growth on leg, foot, or toes
- Color changes in your skin Leg cramps in calves or thighs
- Foot pain
- Painful or tired legs while walking
- Slower walking pace
If you are experiencing any of these symptoms, do not ignore them. Search for a PAD doctor near you.
How is PAD diagnosed?
PAD is diagnosed based on medical and family histories, a physical exam, and test results. Diagnoses from test results include measurements of:
Ankle Brachial Indexes
An Ankle Branchial Index (ABI) test is done by measuring blood pressure at the ankle and in the arm while a person is at rest. Measurements are usually repeated at both sites after five minutes of walking on a treadmill. This can help determine the presence and severity of PAD.
Pulse Volume Recordings
A Pulse Volume Recording (PVR) exam is a non-invasive test that is designed to measure the volume of arterial blood flow (circulation) in the legs or arms. It is similar to a blood pressure exam where cuffs are inflated twice to measure blood volume and blood pressure in an artery.
Ultrasounds
Your physician may also decide to perform a Doppler ultrasound test to determine if a specific artery is open or blocked. This test uses sound waves to measure the blood flow to the veins and arteries in the arms and legs.
What are your Treatment Options?
The overall goals for treating PAD are to reduce symptoms, improve quality of life and mobility, and prevent heart attack, stroke, and amputation. Your health care provider will determine which of the PAD treatment options is best for you, based on your medical history and the severity of your condition.
There are three main approaches to treating PAD:
- Making lifestyle changes
- Taking medication
- Having a procedure performed
Making Lifestyle Changes
 Frequently, PAD can be treated simply by making changes to your lifestyle. For example, quitting smoking and exercising may be all that are needed to relieve PAD symptoms and prevent further progression of the disease.
Frequently, PAD can be treated simply by making changes to your lifestyle. For example, quitting smoking and exercising may be all that are needed to relieve PAD symptoms and prevent further progression of the disease.
Taking Medication[2]
Aspirin or other similar medications may prevent the development of some complications that stem from PAD.
Having a procedure performed
There are several minimally invasive, non-surgical options to treat PAD.
- Arteriogram
An arteriogram is an imaging test that uses x-rays and a contrast agent (sometimes referred to as “dye”) to see inside arteries. - Angioplasty and Stenting
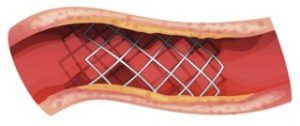 Angioplasty is used to help open narrowed arteries. This technique uses a very small balloon attached to a thin catheter, which is inserted into a blood vessel through a small nick in the skin. The catheter is threaded, under x-ray guidance, to the site of the blockage then the balloon is inflated to open the artery. Sometimes, a small metal scaffold, called a stent, is inserted to keep the blood vessel open.
Angioplasty is used to help open narrowed arteries. This technique uses a very small balloon attached to a thin catheter, which is inserted into a blood vessel through a small nick in the skin. The catheter is threaded, under x-ray guidance, to the site of the blockage then the balloon is inflated to open the artery. Sometimes, a small metal scaffold, called a stent, is inserted to keep the blood vessel open. - Atherectomy
An atherectomy is a minimally-invasive method for treating PAD that removes the plaque within the vessel. The advantages of atherectomy are less vessel trauma, no foreign object left in the body, and future treatment options are open for the patient.
Peripheral artery disease is a serious condition that tends to get overlooked. It is a treatable blockage of the blood vessels that will worsen over time if ignored, increasing the risk of a reduced quality of life, pain, reduced mobility, invasive treatments, gangrene, amputation, or death. To stay comfortable, mobile, and healthy, be proactive and seek out a PAD specialist to evaluate your personal risk for PAD and get screened at the first sign of the previously described symptoms.
Sources:
[1] https://www.nhlbi.nih.gov/health/educational/pad/docs/pad_extfctsht_general_508.pdf
[2] Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): Circulation. 2006; 113:e463-654.