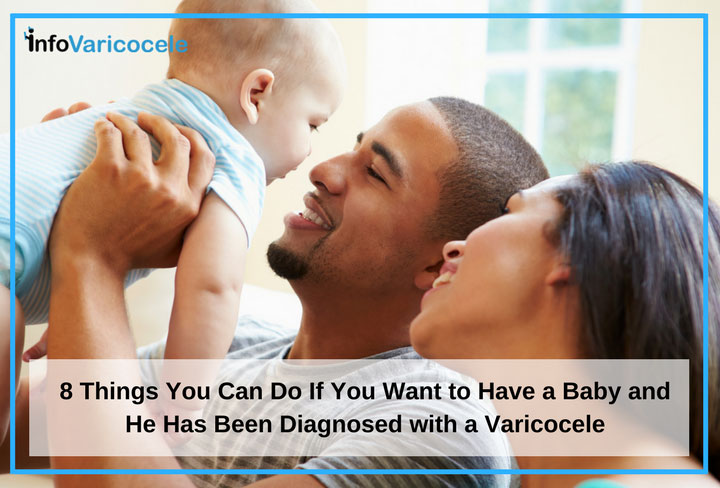
You thought by now you’d have a baby. But after his varicocele diagnosis, you may be wondering if you’ll ever be able to get pregnant. You’re probably thinking about things like What is varicocele related infertility? Is a varicocele treatable? Can we get pregnant? How can I help him? It’s natural to want more answers.
Some Basic Facts About Varicoceles
A varicocele is a collection of dilated blood vessels in the scrotum and around the testicles. About 15% of men have varicoceles, and in about 40% of couples experiencing infertility, a varicocele is a contributing factor.[i,ii] Infertility is when a couple has been trying to get pregnant for 12 months but have not been successful.
Varicoceles are treatable, and the diagnosis doesn’t necessarily mean that you won’t be able to have the baby you want. It’s important that you focus on understanding as much as you can about varicocele related infertility and learn all you can about how to help your partner. Together, you can get through this.
Here’s a list of things you can do that will help you understand varicocele related infertility and how to treat it.
8 Things to Do After a Varicocele Diagnosis
- Listen to him – It’s not uncommon for a man to find it difficult to share his feelings, after a varicocele diagnosis. You shouldn’t force him into talking about his feelings, but if he is open, then listen. Men with varicocele related infertility often feel they did something wrong. Doctors don’t know why varicoceles develop in some men but not others, but for the most part, a varicocele is not preventable. If your partner is having trouble accepting this, then reassure him. Also, it’s ok to remind him that this is treatable.
- Share your feelings – If he asks how you are feeling, you should be honest. You may be feeling disappointment that things aren’t happening as easily as you would like them to. You may be struggling with feelings of hopelessness. If you’re worried that he will be overwhelmed by your feelings, you may want to find a close friend or family member to talk to. You might learn that several of your friends have had fertility challenges as well. Try to remember that varicoceles are treatable.
 Get more information about varicocele treatment options – This point deserves to be emphasized again: varicoceles are a treatable condition. There is a surgical option known as varicocelectomy. This involves one or more incisions to find and tie off the blood vessels causing the varicocele. Surgery can be performed with an open approach, through an incision in the groin, with a microsurgical approach, which involves a microscope, or laparoscopically, with several small incisions for a scope and other surgical equipment.
Get more information about varicocele treatment options – This point deserves to be emphasized again: varicoceles are a treatable condition. There is a surgical option known as varicocelectomy. This involves one or more incisions to find and tie off the blood vessels causing the varicocele. Surgery can be performed with an open approach, through an incision in the groin, with a microsurgical approach, which involves a microscope, or laparoscopically, with several small incisions for a scope and other surgical equipment.
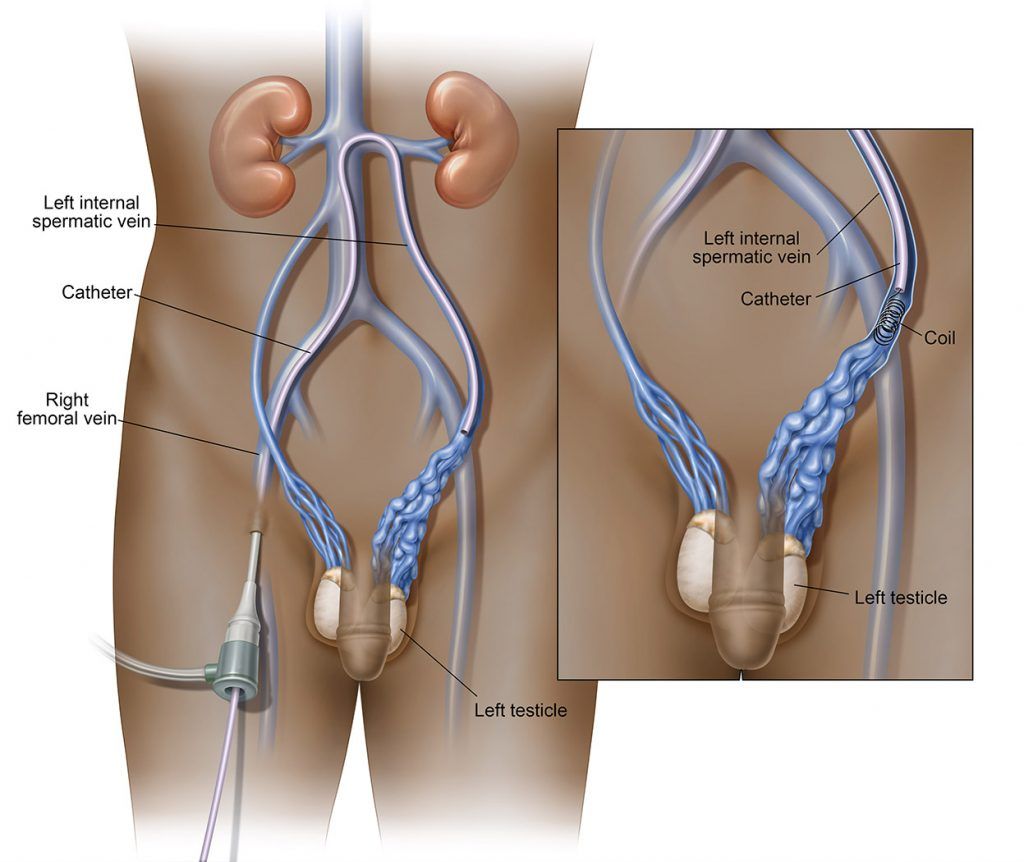
Surgery is not the only treatment; varicocele embolization is a non-surgical, minimally invasive option performed by an interventional radiologist. Through a small nick in the groin, a catheter is inserted. Using x-rays to guide the catheter, the blood vessels causing the varicocele are located and sealed off.- Research the success of each varicocele treatment – Not all treatments are equally effective. Among the surgical treatments, microsurgical varicocelectomy has the best success rate. Varicocele embolization has a success rate of 90%.[iii]
- Research the risks of varicocele surgery – Any procedure or surgery will come with some risk, including potential bleeding and/or infection at the incision site. Varicocele surgery comes with the added risk of hydrocele, which is the development of fluid collecting in the scrotum. Another possible complication is testicular artery ligation, which can compromise the function of the testicle. Laparoscopic varicocelectomy has the added risk of general anesthesia which can cause confusion, nausea and vomiting. General anesthesia is overall very safe, with most people being able to undergo it without any complications.
- Get information about the risks of varicocele embolization – There is virtually no risk of hydrocele or testicular artery ligation with varicocele embolization.[iii] The only anesthesia needed is usually a small amount of a local anesthetic. There is a small risk of bleeding and infection, which is present with any procedure.
- Find out about the chance of pregnancy after treatment – Pregnancy is possible after varicocele treatment. An improvement in the health of and total number of sperm can be seen within 3 months after treatment.[iv] Following varicocelectomy, 26-43% of couples become pregnant. The pregnancy success rate after varicocele embolization is 30-50%.[v]
 Find an interventional radiologist – Look for an interventional radiologist in your area who specializes in the use of varicocele embolization as a treatment for varicocele related infertility. Review the doctor’s website and see if the information provided closely matches your own research. Set up a consultation to discuss this option in greater detail.
Find an interventional radiologist – Look for an interventional radiologist in your area who specializes in the use of varicocele embolization as a treatment for varicocele related infertility. Review the doctor’s website and see if the information provided closely matches your own research. Set up a consultation to discuss this option in greater detail.
Varicoceles can be treated. Listen openly to your partner’s feelings, and share your own thoughts, feelings and concerns. You should feel empowered to help him figure out what can be done to help you have the baby you both want.
Sources:
i Choi, W., and Kim, S., Current Issues in Varicocele Management: A Review. World J Mens Health, 2013. 31(1): p. 12-20. http://wjmh.org/DOIx.php?id=10.5534/wjmh.2013.31.1.12 (accessed 7/31/16).
ii American Society for Reproductive Medicine, Male Infertility. http://www.reproductivefacts.org/topics/detail.aspx?id=1331 (accessed 7/31/2016)
iii Kupis, L., Dobronski, P.A., Radziszewski, P., Varicocele as a source of male infertility – current treatment techniques, Cent European J Urol, 2015. 68: p. 365-370. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4643713/ (last accessed 7/31/2016)
iv Al-Adl, A.M., El-Karamany, T., Issa, H., Zaazaa, M., The influence of antisperm antibodies, intratesticular haemodynamics and the surgical approach to varicoceletomy on seminal variables. Arab Journal of Urology, 2014, 12(4): p. 309-317. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4435656/ (accessed 8/18/2016)
v Cantoro, U., Polito, M., Muzzonnigro, G., Reassessing the role of subclinical varicocele in infertile men with impaired semen quality: a prospective study. Urology, 2015, 85(4): p. 826-30. http://www.ncbi.nlm.nih.gov/pubmed/25817105 (accessed 8/4/2016)