Many women assume that heavy bleeding or severe pelvic pain is just part of their regular menstrual cycle. These symptoms may be a sign of uterine fibroids. Fibroids are noncancerous growths that usually don’t cause any serious health risks, but they can still cause distressing symptoms. For some women, fibroid-related pain can be devastating and impact quality of life. In some cases, fibroids may even affect fertility. So, how are uterine fibroids diagnosed? Read on to learn about uterine fibroids and how to handle a uterine fibroid diagnosis.
What Are Uterine Fibroids?
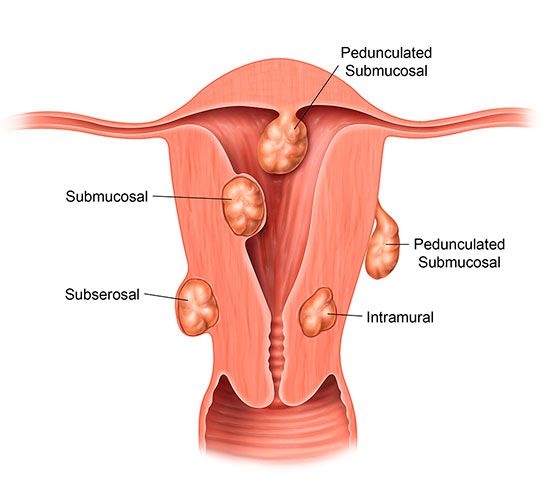
Uterine fibroids are tumors or growths that develop in or around the uterus. The size, shape, and location of fibroids can vary. They’re usually benign, and most fibroids are not linked to an increased risk of uterine cancer (i).
Fibroid symptoms can sometimes be vague. Many women with fibroids are asymptomatic and don’t experience any fibroid-related pain or health problems. You may not realize that symptoms like backaches or constipation can suggest a gynecological problem. Bleeding due to fibroids may also go unnoticed if you’re used to having heavy periods each month. Other women may suffer from severe pain, bleeding, or even infertility (i).
Signs and symptoms of uterine fibroids may include:
- Heavy menstrual bleeding (ii)
- Pelvic pressure or pain (i)
- Frequent urination (ii)
- Difficulty emptying bladder (i)
- Pain during intercourse (ii)
- Constipation (i)
- Backaches (i)
- Leg pain (i)
If you notice any new or worsening symptoms, it’s important to discuss them with your doctor as soon as possible. Your doctor can help determine the exact cause of your symptoms.
How Are Uterine Fibroids Diagnosed?
Fibroids are sometimes diagnosed during a routine pelvic exam.
If the results of your pelvic exam suggest fibroids, your doctor may order an ultrasound. This noninvasive test uses sound waves to create a picture of your reproductive organs (iv).
In some cases, an ultrasound may not provide enough information. Your doctor may recommend additional imaging studies, including: (iv)
- MRI
- Hysterosonography
- Hysterosalpingography
- Hysteroscopy
These imaging tests are usually performed in an outpatient setting. They can help your doctor gather the information needed to develop a uterine fibroid treatment plan. You may need several tests before your doctor can determine the right treatment strategy.
What Causes Uterine Fibroids?
Doctors aren’t exactly sure what causes fibroids, but some women seem to be at a higher risk than others. Potential risk factors can include:
- Obesity (ii)
- Poor diet (i)
- Vitamin D deficiency (i)
- Family history of fibroids (ii)
- Early onset of menstruation (i)
Fibroids are affected by the hormone levels in your body. High levels of estrogen seem to cause fibroids to grow larger. Meanwhile, some antihormonal drugs can work to shrink fibroids (ii). Taking certain hormonal medications, like hormone replacement therapy, may increase your risk of developing fibroids (iii).
Certain racial groups also seem to be more likely to develop fibroids. For example, African-American women are at a higher risk for uterine fibroids than women from other ethnicities (ii). Your doctor can help you determine whether you’re at risk for fibroids.
Fibroids and infertility
Many women with fibroids go on to have healthy pregnancies (ii) but some fibroids can cause fertility problems. Large fibroids may distort the shape of the uterus or cause abdominal swelling. Other types of fibroids can prevent a fertilized egg from attaching to the uterine wall (v).
Some women with fibroids are at higher risk for miscarriage or post-birth complications (ii). If you have fibroids, it’s essential to get an accurate diagnosis as soon as possible. Once your doctor determines the size, number, and location of your fibroids, he or she can help you choose the right treatment plan.
A Minimally Invasive Treatment Option
Treatment for fibroids can range from no treatment to surgery to a minimally invasive outpatient procedure. If your fibroids are small and asymptomatic, treatment usually isn’t necessary. (iv) If your fibroids are large, painful, or causing fertility problems, treatment may be needed.
It’s important to understand that not all women with uterine fibroids require invasive surgery and hospitalization. Hysterectomy is no longer the only treatment available for fibroids (iv). Fibroid treatment options now include a variety of minimally invasive and noninvasive procedures which can offer relief from fibroid symptoms while preserving your uterus.
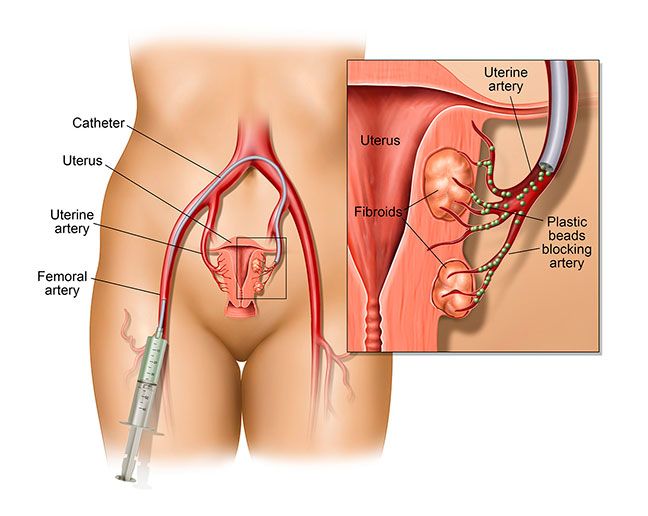
Uterine fibroid embolization (UFE) is a minimally invasive, outpatient procedure and an alternative to open surgery. UFE blocks blood flow to the fibroid(s), causing them to shrink and die. UFE provides up to 90 percent of patients with significant symptom relief (vi) such as decreased menstrual bleeding and symptoms of pain, pressure, urinary frequency or constipation.
UFE can be performed in an outpatient vascular center or an ASC, rather than a hospital based operating room, by an interventional radiologist or vascular specialist. You will be sedated for the procedure, so you will remain awake, but not fully alert.
The vascular specialist will place a needle in a femoral or transradial artery. A small catheter is then advanced into the artery, or arteries, that supplies blood to the fibroids. The catheter is then used to slowly inject tiny, medical-grade synthetic particles, which are the size of a grain of sand. These tiny particles block blood flow in the affected artery, causing fibroids to shrink (vi). When blood flow to the fibroid is blocked, the fibroid no longer receives oxygen and nutrients, and over time, will begin to die.
Once the UFE procedure is completed, you must rest in bed, lying flat with your leg straight.
When you’re cleared to go home, you will continue to recover in the comfort of your own home.
At Azura Vascular Care, UFE is performed by a highly trained vascular specialist. The staff provides expert care in a fully equipped outpatient setting. There’s no need to wait for hours in a crowded hospital waiting room. Azura Vascular Care offers a variety of procedures and follow-up care in one convenient location.
Ready to learn more about UFE? Download our free information sheet, Understanding Uterine Fibroid Embolization (UFE), or call 844-UFE-CARE (833-2273) today to schedule an appointment with a vascular specialist.
Sources:
(i) Mayo Clinic. (2018, March 6). Uterine fibroids: Symptoms & causes. Retrieved December 7, 2018, from https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/symptoms-causes/syc-20354288.
(ii) U.S. Department of Health & Human Services: Office on Women’s Health. (2018, March 16). Uterine fibroids. Retrieved December 7, 2018, from https://www.womenshealth.gov/a-z-topics/uterine-fibroids.
(iii) Medical News Today. (2017, September 30). Fibroids after menopause: What you need to know. Retrieved December 7, 2018, from https://www.medicalnewstoday.com/articles/319576.php.
(iv) Mayo Clinic. (2018, March 6). Uterine fibroids: Diagnosis & treatment. Retrieved December 7, 2018, from https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/diagnosis-treatment/drc-20354294.
(v) UCLA Health. Infertility. Retrieved December 10, 2018, from http://obgyn.ucla.edu/infertility.
(vi) RadiologyInfo. (2018, February 25). Uterine Fibroid Embolization (UFE). Retrieved December 7, 2018, from https://www.radiologyinfo.org/en/info.cfm?pg=ufe.